Revolutionizing Healthcare: How AI Ambient Voice Technology Eases Physician Burnout and Boosts Patient Satisfaction
Healthcare systems around the world are grappling with two parallel crises that are deeply intertwined yet often addressed in isolation: the growing epidemic of physician burnout and the rising tide of patient dissatisfaction. As healthcare becomes increasingly complex and digitized, frontline medical professionals find themselves burdened by administrative overload, while patients struggle with impersonal care experiences that erode trust and satisfaction. This convergence of clinician distress and consumer discontent threatens not only the quality of care but also the long-term sustainability of healthcare delivery.
Physician burnout has reached alarming levels, with surveys consistently showing that over 60% of doctors in certain specialties report symptoms of burnout. These symptoms—emotional exhaustion, depersonalization, and a diminished sense of personal accomplishment—are not merely workplace grievances. They are precursors to serious consequences such as increased medical errors, lower patient safety, and higher attrition rates. Alarmingly, the root cause is not always clinical pressure but rather the burden of documentation, coding, and clerical responsibilities—tasks that consume up to half of a physician’s workday and extend into after-hours, commonly referred to as “pajama time.”
Simultaneously, patients are reporting a decline in the quality of their interactions with healthcare providers. In many clinical settings, patients now encounter physicians who are more focused on screens than on their narratives. The erosion of face-to-face communication—once the hallmark of compassionate care—has tangible consequences: reduced trust, incomplete histories, and overall dissatisfaction with the healthcare experience. With healthcare systems emphasizing patient-centric care, this gap between expectation and reality demands urgent attention.
In this context, artificial intelligence (AI) emerges not merely as a technological novelty but as a transformative solution. Specifically, AI-powered ambient voice capture systems are being hailed as a critical tool for relieving the administrative burden on clinicians while simultaneously improving patient engagement. By passively listening and documenting medical conversations during consultations, these systems enable physicians to remain fully present with their patients, reclaim their time, and produce higher quality clinical documentation. Unlike traditional dictation tools, ambient voice AI operates in the background, capturing relevant context and synthesizing structured notes without disrupting the natural flow of conversation.
The implementation of ambient voice capture technologies represents a shift in the clinical paradigm—from manual data entry to AI-assisted documentation. This shift promises to rehumanize healthcare by allowing clinicians to focus on what they do best: listening, diagnosing, and healing. Furthermore, the data generated by these systems can support broader quality improvement initiatives, from performance analytics to population health management.
In recent years, major players such as Microsoft’s Nuance DAX, Abridge, Suki, and DeepScribe have made significant strides in deploying ambient voice technologies across hospitals and outpatient settings. These tools leverage sophisticated natural language processing (NLP), machine learning, and speech recognition models to understand medical discourse, identify key elements of clinical encounters, and populate electronic health records (EHRs) with unprecedented accuracy and efficiency. Their impact is already being felt, with early adopters reporting substantial reductions in documentation time and notable increases in physician satisfaction.
Yet, as with any technological advancement in medicine, ambient voice AI is not without its critics or challenges. Issues of data privacy, error correction, legal liability, and the need for patient consent must be rigorously addressed. Moreover, equitable access to these technologies remains a concern, especially in under-resourced healthcare settings. Nonetheless, the momentum behind AI-driven ambient voice capture is accelerating, fueled by compelling evidence and the urgent need for systemic relief.
This blog post explores the promise and complexity of ambient voice capture technology in healthcare. It begins by unpacking how the technology works and the AI innovations that power it. It then evaluates its impact on physician burnout, delves into the patient experience, and finally examines ethical considerations and future directions. By the end, readers will understand how AI is reshaping the healthcare encounter—and why this transformation matters more than ever in an era of both crisis and opportunity.
Understanding AI Ambient Voice Capture Technology
The integration of artificial intelligence into clinical workflows is revolutionizing how healthcare is delivered, documented, and optimized. Among the most impactful innovations in this space is AI-powered ambient voice capture—a technology that passively records, interprets, and transcribes conversations between physicians and patients in real time. Unlike traditional voice dictation tools that require direct engagement and structured commands, ambient voice AI operates unobtrusively in the background, seamlessly transforming natural dialogue into structured, actionable clinical documentation. This section provides an in-depth examination of how ambient voice capture technology functions, the core components of its architecture, the major players in the industry, and the growing relevance of this innovation in modern medicine.
Defining Ambient Voice Capture in Healthcare
Ambient voice capture in the clinical context refers to systems that automatically listen to and interpret conversations occurring during medical encounters, typically between a healthcare provider and a patient. These systems are designed to integrate unobtrusively into the clinical setting—through smart microphones, mobile apps, or embedded devices—without requiring users to change their natural speech patterns or manually interact with the system during consultations. The objective is to replicate the functionality of a human medical scribe, capturing essential elements such as symptoms, history, assessments, diagnoses, and care plans, while minimizing interruptions to the patient-provider interaction.
Unlike standard voice-to-text transcription tools, which simply record and transcribe verbatim speech, ambient AI systems leverage advanced natural language processing (NLP), contextual understanding, and machine learning to distinguish between clinically relevant information and conversational noise. This allows them to generate structured notes that comply with medical documentation standards and are compatible with electronic health record (EHR) systems.
Key Components and Technologies
At the heart of ambient voice capture lies a sophisticated interplay of artificial intelligence disciplines:
- Automatic Speech Recognition (ASR): Converts spoken language into raw text. ASR models must be capable of handling various accents, medical terminology, and overlapping speech.
- Natural Language Processing (NLP): Interprets meaning from the raw text, identifying clinical entities such as symptoms, medications, and diagnoses.
- Contextual Analysis: Determines speaker roles (e.g., physician vs. patient), identifies conversational intent, and distinguishes medically relevant content.
- Summarization Engines: Condense long dialogues into coherent clinical summaries suitable for EHR integration.
- Integration APIs: Connect the ambient capture platform with EHRs such as Epic, Cerner, or Allscripts to populate fields like SOAP (Subjective, Objective, Assessment, Plan) notes.
These systems are designed to learn continuously, improving their transcription accuracy, clinical relevance, and contextual intelligence over time. Many ambient AI platforms also incorporate human-in-the-loop (HITL) workflows, where human reviewers audit or edit AI-generated notes to ensure clinical accuracy and compliance.
Deployment Models and Workflows
Ambient voice capture systems can be deployed in several formats depending on the clinical environment:
- On-Premise Devices: Hardware devices installed in examination rooms that capture and process voice locally.
- Mobile Applications: Smartphone-based systems that record and upload voice data to cloud services for processing.
- Cloud-Connected Microphones: Devices like Nuance’s Dragon Ambient eXperience (DAX) that link with secure cloud platforms for processing and EHR entry.
- Telemedicine Integration: Captures conversations during virtual consultations, often through existing video conferencing platforms.
These tools are built with strict compliance to data protection laws such as HIPAA in the United States, ensuring that patient privacy is preserved at all times. Voice data is typically encrypted, anonymized when necessary, and processed under secure conditions with strict access controls.
Leading Platforms and Market Landscape
Several technology providers have emerged as leaders in ambient voice capture for healthcare:
- Nuance DAX (by Microsoft): Perhaps the most widely recognized, DAX captures multi-party conversations and generates structured clinical documentation integrated directly into EHR systems. Its AI is trained on millions of medical conversations and refined with HITL review.
- Abridge: Focused on patient-centered communication, Abridge emphasizes transparency by offering summaries to both physicians and patients post-consultation.
- Suki AI: Offers voice-enabled assistants that combine dictation, ambient capture, and AI-generated note creation in one platform.
- DeepScribe: Markets itself as a low-friction solution for small practices, offering plug-and-play ambient scribing with HITL validation.
- Augmedix: Originally focused on live medical scribes, now incorporates AI voice capture to reduce the need for human scribes in real time.
These platforms differentiate themselves based on their specialization (primary care, specialty care, telehealth), the degree of automation vs. human review, multilingual support, and the depth of EHR integration.
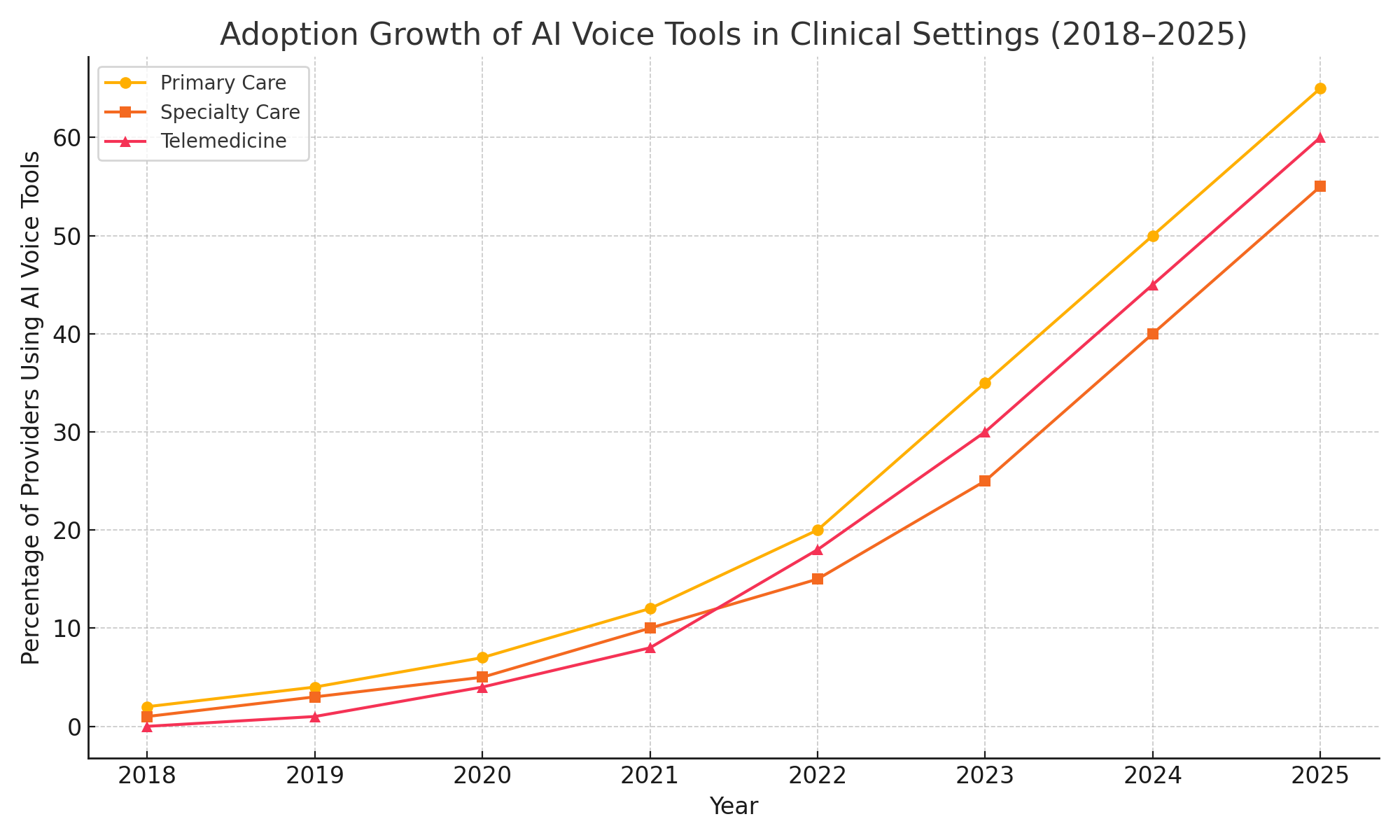
Adoption Drivers and Value Proposition
The growing adoption of ambient voice AI in healthcare is driven by several converging factors:
- Documentation Burden: Physicians spend up to two hours on EHR tasks for every one hour of direct patient care. Ambient voice systems alleviate this pressure by automatically capturing key elements of the visit.
- Clinical Efficiency: Automating note creation allows for faster patient throughput and improved clinic workflow.
- Reimbursement and Coding Accuracy: AI-generated documentation helps ensure accurate and complete coding, which can improve revenue cycle outcomes.
- Patient Experience: Eliminating the need for physicians to multitask during appointments leads to more engaged, personal encounters.
Early reports from hospitals implementing these systems indicate that physicians save between 6 to 10 hours per week in administrative tasks, with documentation times reduced by up to 70%. Many users also report improvements in documentation quality and fewer documentation-related errors.
The Role of EHR Integration
A critical enabler of ambient voice AI is seamless integration with existing electronic health record systems. Without this, the benefits of AI documentation are significantly diminished. Integration ensures that structured notes flow directly into patient charts, eliminating duplicate work and ensuring clinical continuity. Leading platforms offer plug-ins or APIs for popular EHRs, enabling real-time data synchronization, editing capabilities, and compliance with institutional documentation policies.
Moreover, advanced platforms can auto-populate fields such as review of systems (ROS), history of present illness (HPI), physical exam findings, and even clinical orders based on physician commands or conversation context. This transforms documentation from a manual burden into an automated value-adding process.
Conclusion
AI ambient voice capture technology is more than a speech-to-text convenience—it is an intelligent system engineered to enhance the quality, speed, and integrity of clinical documentation. Through a combination of real-time processing, contextual understanding, and robust integration with EHR platforms, these tools are redefining the clinical encounter. As adoption increases and the technology matures, ambient AI is poised to become an indispensable asset in modern healthcare, addressing the systemic pain points of burnout and documentation overload.
Alleviating Physician Burnout: Evidence and Outcomes
Physician burnout has emerged as one of the most pressing public health crises in modern medicine. Characterized by chronic emotional exhaustion, detachment from patients, and a diminished sense of professional efficacy, burnout impacts nearly every facet of healthcare delivery. Studies consistently report that over half of U.S. physicians experience at least one symptom of burnout. The consequences are multifaceted: decreased job satisfaction, reduced productivity, compromised patient care, and increased physician turnover. Central to this challenge is the administrative burden placed on clinicians—particularly the overwhelming demands of electronic health record (EHR) documentation.
Artificial intelligence (AI)-powered ambient voice capture offers a tangible remedy. By relieving clinicians of the need to manually record and organize their clinical notes, this technology significantly reduces cognitive load, restores work-life balance, and enhances clinical efficiency. This section delves into the empirical and anecdotal evidence supporting the positive impact of ambient voice AI on physician burnout, including real-world case studies, before-and-after metrics, and key outcomes reported by early adopters.
Burnout and Documentation: A Causal Relationship
At the core of the burnout epidemic is a fundamental misalignment between physicians' responsibilities and their core motivations. Most physicians enter the profession to care for patients—not to spend hours performing clerical tasks. However, data from the American Medical Association (AMA) and other sources reveal that physicians spend over 50% of their workday interacting with EHRs and performing documentation tasks. An additional 1 to 2 hours per evening is often spent completing notes from earlier in the day, a phenomenon known as “pajama time.” This extended screen time correlates strongly with increased rates of burnout, dissatisfaction, and early retirement.
Ambient voice capture solutions are designed to address this imbalance directly. By passively listening to clinical conversations and automatically generating encounter documentation, these tools effectively offload one of the most significant administrative burdens from the physician’s shoulders. The ability to reclaim time—during and after clinic hours—has been consistently linked to improvements in physician well-being.
Quantifying Time Savings and Efficiency Gains
Numerous pilot programs and implementation studies across hospitals and clinics have demonstrated substantial time savings through ambient voice capture. In a 2023 study conducted by a large academic health system using Nuance DAX, physicians reported an average reduction of 7 hours per week in documentation time. Across multiple specialties, clinicians noted a 30% to 70% decrease in charting tasks, depending on their patient volume and complexity.
A similar study published by the American College of Physicians highlighted that family medicine practitioners using Suki AI saved 3 to 4 minutes per patient in documentation time, amounting to over 1 hour saved per clinic day. These time gains translate into tangible benefits: the ability to see more patients, end the day on time, or simply recover personal hours previously lost to clerical work.
The following table provides an overview of before-and-after metrics reported by physicians using ambient AI systems:
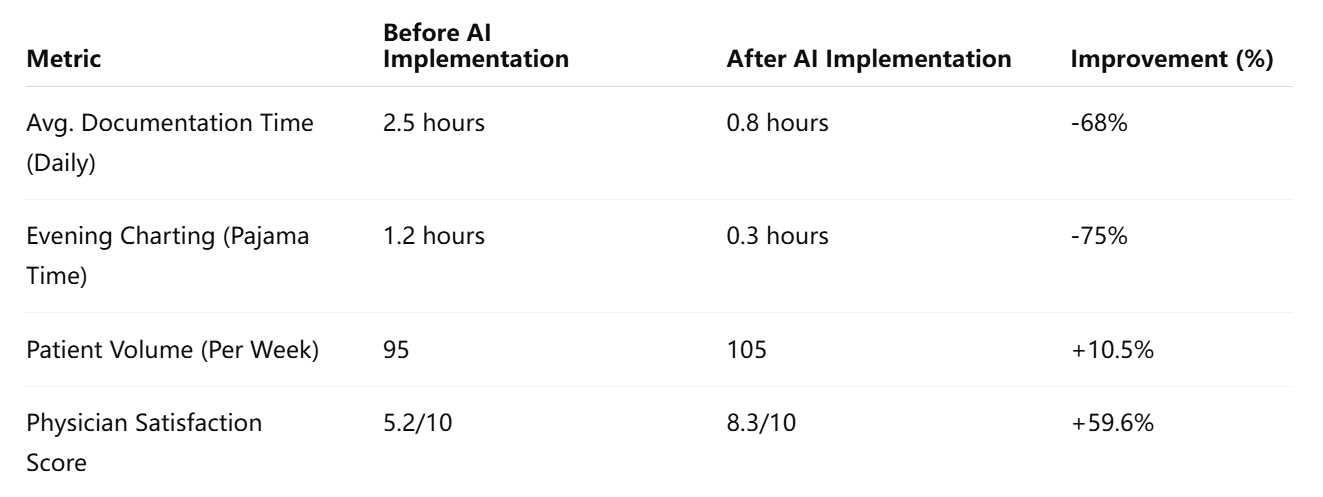
These metrics suggest that AI voice assistants not only reduce workload but also enhance the overall clinical experience for providers. Time saved from documentation duties can be reinvested in patient care, medical education, research, or self-care—each of which contributes to a more sustainable practice environment.
Reducing Emotional Exhaustion and Cognitive Load
Burnout is not only a product of long hours—it is also a function of how those hours are spent. Repetitive, low-value tasks such as documentation drain physicians’ mental energy and shift their focus away from meaningful patient interaction. By handling note-taking in the background, ambient voice AI allows clinicians to concentrate more fully on diagnostic reasoning, clinical problem-solving, and relational communication.
Psychologically, the benefits are profound. In interviews with clinicians using ambient capture tools, many describe a renewed sense of presence and attentiveness in the exam room. Eye contact with patients improves. Conversations become less transactional. The “invisible wall” created by typing into a computer during patient encounters begins to dissipate.
One internal medicine physician at a major urban hospital reported:
“For the first time in years, I felt like I could listen without multitasking. I wasn’t dividing my attention between the patient and the computer—I was just being a doctor.”
This re-engagement with the human side of medicine plays a critical role in mitigating emotional exhaustion and fostering professional fulfillment.
Burnout Reduction Across Specialties
While all physicians stand to benefit from reduced documentation demands, certain specialties have shown particularly strong results with ambient voice AI:
- Primary Care: High patient volumes and short visit durations make time savings especially impactful. Clinicians in family medicine and internal medicine report rapid efficiency gains.
- Emergency Medicine: Fast-paced environments benefit from real-time note generation and reduced charting delays.
- Behavioral Health: Extended conversations require nuanced documentation; ambient tools are well-suited to capturing these interactions.
- Orthopedics and Surgical Subspecialties: Procedural note automation accelerates post-operative documentation.
Each specialty presents unique workflow requirements, and AI vendors are increasingly customizing their models to address specialty-specific lexicons, terminologies, and encounter types.
Case Studies and Testimonials
A growing number of healthcare institutions have implemented ambient voice solutions with measurable success:
- Atrium Health (USA): Implemented Nuance DAX across multiple departments. Physicians reported a 70% reduction in documentation time and a 90% satisfaction rate with the tool.
- Mayo Clinic: Piloted ambient AI for primary care providers. Early results indicate increased note accuracy and improved coding compliance, along with a decrease in physician-reported burnout.
- National Health Service (UK): In select trusts, AI voice capture is being explored as part of a digital transformation strategy to retain clinical staff and streamline documentation.
The common theme across these deployments is the restoration of time and attention—two of the most valuable yet scarce resources in medicine.
Conclusion
AI-powered ambient voice capture is proving to be a critical intervention in the fight against physician burnout. By automating documentation, it relieves clinicians of one of their most significant administrative burdens, enabling them to focus on high-value, human-centered care. The evidence—ranging from reduced documentation times to improved job satisfaction—indicates that this technology does not merely streamline workflow but restores purpose to clinical practice. In the next section, we explore how ambient AI impacts patient satisfaction and transforms the clinical encounter from the patient’s perspective.
Enhancing Patient Satisfaction and Clinical Communication
While physician burnout has rightly commanded attention in the debate over healthcare modernization, the patient experience remains the definitive measure of clinical success. As patients become more informed and healthcare shifts toward value-based models, satisfaction is no longer a secondary concern but a core performance indicator. In this context, AI ambient voice capture systems—initially designed to ease documentation for providers—are now also being recognized for their transformative impact on the quality of patient-provider interactions.
Ambient voice AI restores the centrality of human connection in healthcare. By automating documentation and freeing clinicians from the tyranny of keyboards and screens, these technologies empower physicians to focus on listening, empathizing, and engaging. This section explores how ambient voice capture enhances patient satisfaction, supports clearer clinical communication, and contributes to a more compassionate, efficient care experience.
Reclaiming the Physician’s Attention
Perhaps the most immediate and visible benefit of ambient voice AI is the restoration of eye contact and face-to-face communication during medical visits. In traditional settings, physicians often divide their attention between patients and their computers—typing, clicking, and navigating complex EHR interfaces. This multitasking, while necessary, dilutes the quality of the interaction and signals to patients that they are not the focal point of the encounter.
Ambient voice capture allows physicians to engage in conversation without the need to take manual notes. As the AI listens and transcribes in the background, the clinician is free to maintain continuous engagement. Studies show that patients interpret this increased attention as a sign of respect, empathy, and professionalism—all of which are directly correlated with higher satisfaction scores.
According to a 2023 survey by the American Academy of Family Physicians (AAFP), clinics using ambient AI tools saw a 24% increase in patient satisfaction scores within three months of implementation. The most common patient comments referenced “feeling heard,” “not rushed,” and “the doctor looking at me, not the screen.”
Improving the Accuracy and Consistency of Clinical Information
Another benefit of ambient voice capture is its contribution to the accuracy and completeness of the medical record. When physicians are tasked with recalling details after a patient visit—often several hours later—errors and omissions can occur. Ambient AI systems, by capturing conversations in real time, reduce reliance on memory and ensure that critical details are documented with fidelity.
This has several downstream benefits:
- Continuity of Care: Accurate notes support handoffs between providers and improve decision-making during follow-up visits.
- Patient Trust: When patients see that their concerns are remembered and addressed in subsequent encounters, they are more likely to trust their providers.
- Legal Protection: Accurate documentation also helps mitigate the risk of litigation due to miscommunication or incomplete records.
Moreover, some platforms, such as Abridge and DeepScribe, provide patients with post-visit summaries that include the key points discussed during the encounter. These summaries help reinforce instructions, improve adherence to care plans, and reduce confusion—particularly for patients managing chronic conditions or those with language or cognitive barriers.
Promoting Transparency and Empowerment
Ambient AI tools are not just provider-facing technologies; they increasingly serve as instruments of patient empowerment. By generating and sharing structured visit summaries, these tools offer patients the opportunity to review, reflect on, and clarify what was said during their consultations.
This transparency supports a broader shift toward collaborative care models, where patients are active participants rather than passive recipients. For example, a patient managing type 2 diabetes may receive a visit summary outlining dietary guidance, medication adjustments, and follow-up schedules—all of which can be easily referenced after the appointment. Such summaries reduce dependence on memory and facilitate informed decision-making.
Furthermore, multilingual and accessibility-focused platforms are making it possible to tailor visit summaries to different patient populations, including those with limited English proficiency, hearing impairments, or low health literacy. By increasing accessibility, ambient AI tools help reduce disparities in care delivery and information access.
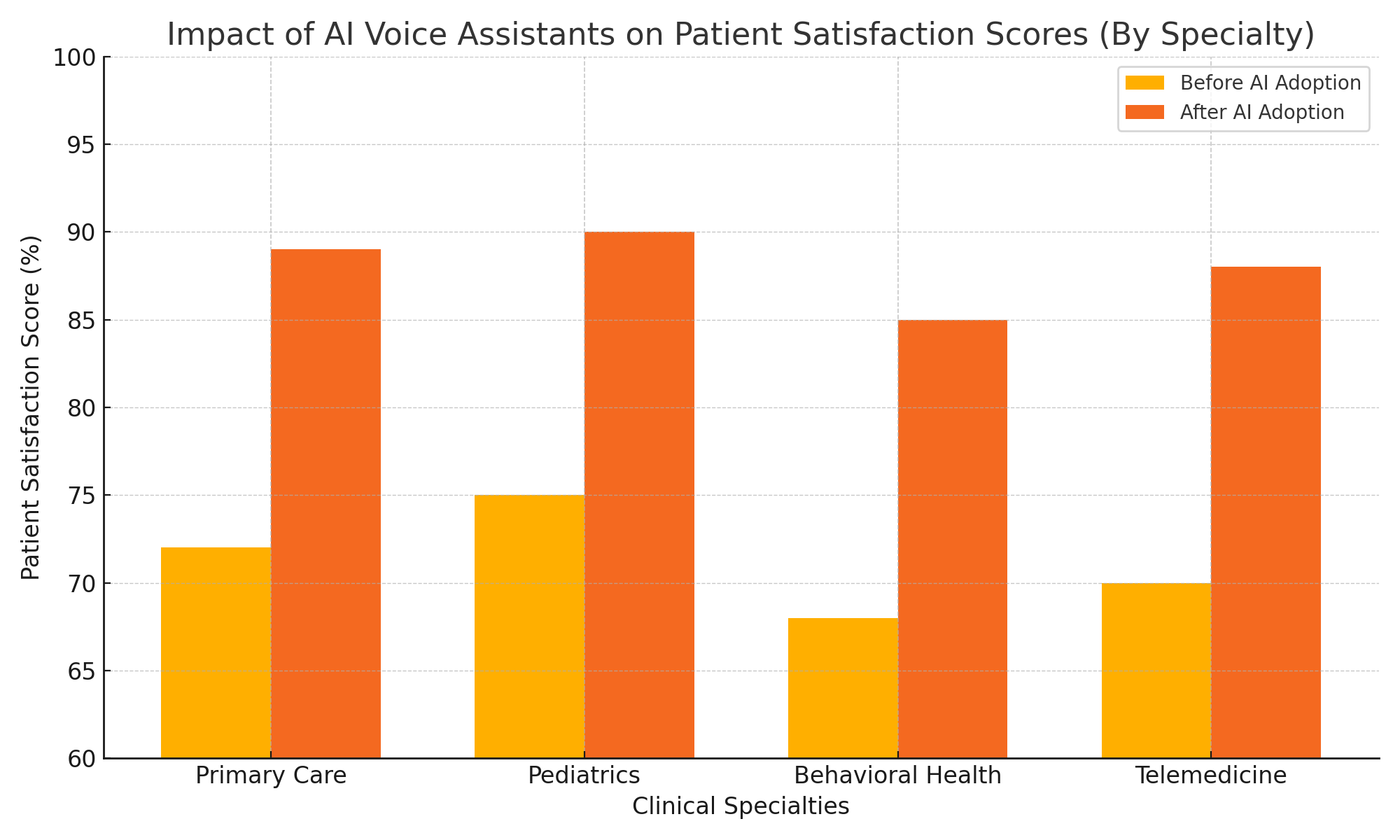
Impact Across Demographics and Specialties
The positive impact of ambient voice capture on patient satisfaction is not limited to any single demographic or clinical context. Evidence suggests that improvements are observed across a wide range of patient groups and specialties.
- Geriatric Patients: Often report better understanding and reduced anxiety when provided with post-visit notes.
- Pediatric Care: Parents appreciate clear documentation of care plans and feel more included in the care process.
- Behavioral Health: Longer, more personal conversations are preserved with nuance, fostering trust and continuity.
- Telemedicine: Ambient AI enhances remote visits by ensuring that nothing gets “lost in translation” over digital interfaces.
Healthcare systems have begun tracking improvements in standardized satisfaction metrics such as the Hospital Consumer Assessment of Healthcare Providers and Systems (HCAHPS) and Press Ganey scores after implementing ambient voice AI. Clinics that adopt these tools often see boosts in ratings related to provider communication, perceived attentiveness, and clarity of discharge instructions.
Enhancing the Patient Narrative
In addition to summarizing data for clinicians, ambient AI systems are also capable of preserving the patient’s narrative in a more authentic and holistic way. Traditional note templates often truncate patient stories into checkbox formats or overly rigid structures. Ambient systems, by capturing the patient’s language and context, maintain narrative integrity—something patients deeply value.
Capturing phrases such as “it started after my vacation” or “it feels like a stabbing pain, especially when I turn my head” can be diagnostically significant. When these details are accurately recorded, they contribute to more precise diagnoses and personalized care plans.
Preserving the patient voice in documentation not only enhances the quality of care but also demonstrates that the clinician is truly listening—an essential component of a positive care experience.
Conclusion
Ambient voice AI technologies are proving to be powerful tools in restoring the humanity of medical encounters. By liberating clinicians from administrative distraction, they enable more present, empathetic, and effective communication. For patients, this translates into improved satisfaction, clearer understanding, and greater trust in their providers. In an era where healthcare systems must balance efficiency with empathy, AI voice capture emerges not as a threat to human connection, but as its enabler. The final section will examine the ethical, operational, and regulatory challenges that must be addressed to ensure that the deployment of this technology benefits all stakeholders.
Barriers, Ethical Considerations, and the Future Outlook
Despite its transformative potential, AI-powered ambient voice capture technology does not exist in a vacuum. As with any innovation in healthcare, its deployment and widespread adoption are subject to a range of operational, ethical, regulatory, and equity-based considerations. While early evidence strongly supports its efficacy in reducing physician burnout and improving patient satisfaction, stakeholders must navigate complex barriers to ensure responsible and effective implementation. This final section critically examines the obstacles that currently hinder broader adoption and outlines the path forward for scaling ambient voice capture responsibly.
Financial and Operational Barriers to Adoption
One of the most immediate challenges in deploying ambient AI tools is the financial investment required. These technologies—especially enterprise-grade systems with robust EHR integration—often come with substantial licensing fees, infrastructure demands, and training costs. For large health systems, these expenses can be justified through long-term gains in physician efficiency, reduced burnout, and improved billing accuracy. However, for small practices and community clinics, the cost barrier can be prohibitive.
Additionally, operational integration can pose difficulties. Implementing ambient voice capture requires technical compatibility with existing EHRs, secure audio capture infrastructure, and reliable internet connectivity. Initial rollouts may also encounter workflow disruptions, as clinicians adapt to the presence of AI systems in the exam room.
Addressing these hurdles will require industry-wide efforts to provide flexible pricing models, interoperable APIs, and streamlined onboarding processes. Vendors that offer scalable and customizable solutions—catering to diverse practice sizes and specialties—are likely to see stronger market traction.
Privacy, Consent, and Data Governance
Given that ambient voice capture systems operate by recording clinical conversations, patient privacy and informed consent are foundational ethical concerns. Compliance with regulations such as the Health Insurance Portability and Accountability Act (HIPAA) in the United States, the General Data Protection Regulation (GDPR) in Europe, and other regional frameworks is non-negotiable.
Key considerations include:
- Explicit Consent: Patients must be fully informed that their conversations are being recorded and transcribed, and they must have the option to opt out without consequence.
- Data Storage and Transmission: All audio and textual data must be encrypted in transit and at rest, with clearly defined data retention policies.
- Access Controls: Only authorized users should be able to view or edit AI-generated notes. Audit trails and user permissions are critical.
- Third-Party Use: Some platforms may use anonymized data to improve model performance. Patients and providers must be aware of and agree to such practices.
To gain and maintain trust, healthcare providers must ensure that AI voice tools are deployed transparently and ethically. Regulatory bodies may soon require formal ethics reviews or certifications for any AI system that processes clinical conversations.
Addressing Algorithmic Bias and Clinical Accuracy
AI systems are not immune to bias. Voice recognition models can underperform when exposed to accents, dialects, or speech patterns not represented in their training data. This has implications not only for equity in documentation quality but also for diagnostic accuracy and billing integrity.
Moreover, clinical transcription is a high-stakes task. Misinterpretations, omissions, or contextual misunderstandings by the AI could result in clinical errors or malpractice risks. While many platforms include a “human-in-the-loop” (HITL) review to mitigate such risks, this layer adds cost and complexity.
To address these issues, vendors must:
- Ensure diverse and inclusive training datasets that reflect real-world demographics.
- Implement validation protocols across multiple specialties and patient populations.
- Allow easy post-editing and feedback loops to improve model accuracy continuously.
Clinician oversight remains essential. AI should serve as an assistant—not a replacement—for clinical judgment and documentation review.
Ethical Design and the Clinician-Patient Dynamic
Another subtle yet critical issue involves the intrusiveness of AI in what should be a private and personal encounter. Even when unobtrusive, ambient microphones may alter patient behavior or inhibit disclosure, particularly for sensitive topics such as mental health, sexual health, or substance use.
Ethical design must prioritize non-intrusiveness, ensuring that ambient systems do not interfere with the therapeutic relationship. This includes:
- Transparent placement of devices.
- Clear audio indicators or visual cues for when recording is active.
- Simple opt-out procedures that don’t degrade the quality of care.
Clinicians must also be trained to set expectations with patients at the beginning of each visit, ensuring that technology supports rather than supplants the human connection.
The Future of Ambient AI in Healthcare
Despite these challenges, the long-term outlook for ambient voice capture in medicine remains highly optimistic. The technology is maturing rapidly, and its benefits are too substantial to ignore. Several trends are expected to shape the future of this domain:
- Multilingual Support: As global healthcare systems embrace AI, tools will evolve to support multilingual and cross-cultural contexts, improving equity in care.
- Clinical Decision Support Integration: Future platforms may not only document conversations but also analyze them for clinical insights, flag potential red flags, and recommend interventions.
- Wearable and Mobile Integration: Ambient AI may expand beyond the clinic into patients’ homes, supporting longitudinal care via smart devices.
- Patient-Facing Applications: Patients could use ambient tools to document symptoms at home, prepare for appointments, or review past visits through conversational interfaces.
Additionally, ambient voice technology may converge with agentic AI systems, enabling voice assistants to schedule follow-ups, request lab tests, or initiate referrals—all autonomously, under clinician supervision.
Conclusion
AI-powered ambient voice capture is not a panacea, but it represents a powerful leap forward in the evolution of healthcare documentation and communication. To unlock its full potential, stakeholders must address critical concerns around cost, ethics, privacy, and fairness. A collaborative approach—bringing together technologists, clinicians, regulators, and patients—is essential to build systems that are both intelligent and humane. If done thoughtfully, ambient voice AI could become not only a remedy for burnout and dissatisfaction, but a foundation for a more connected, compassionate, and effective healthcare system.
References
- Nuance DAX – https://www.nuance.com/healthcare/ambient-clinical-intelligence.html
- Abridge AI – https://www.abridge.com
- Suki AI – https://www.suki.ai
- DeepScribe – https://www.deepscribe.ai
- American Medical Association on Burnout – https://www.ama-assn.org/practice-management/physician-health
- National Academy of Medicine on Clinician Well-Being – https://nam.edu/initiatives/clinician-resilience-and-well-being
- Epic Systems – https://www.epic.com
- HIPAA Privacy Rule Summary – https://www.hhs.gov/hipaa/for-professionals/privacy/laws-regulations/index.html
- AAFP on Patient Satisfaction – https://www.aafp.org
- Press Ganey Patient Experience – https://www.pressganey.com/solutions/patient-experience