Microsoft's Diagnostic AI Outperforms Doctors: A Turning Point in Medical Technology

In a bold declaration that has stirred both excitement and skepticism across the healthcare and technology sectors, Microsoft recently announced that its artificial intelligence (AI) system can outperform human doctors in diagnosing complex medical conditions. This breakthrough marks a pivotal shift in the landscape of modern medicine, where computational power, data-driven insights, and advanced machine learning models are now directly challenging—and potentially complementing—the cognitive capabilities of trained physicians. At the heart of this development lies Microsoft’s commitment to pushing the boundaries of what AI can achieve in clinical environments, not merely as a passive analytical tool, but as an active diagnostic agent with real-world applicability.
The implications of such a claim are far-reaching. Healthcare systems across the globe are under increasing pressure from rising patient volumes, shrinking medical workforces, and the ever-present burden of diagnostic errors—some of which are life-threatening. The introduction of an AI system that not only assists but surpasses the diagnostic accuracy of experienced physicians signals a potential paradigm shift in how medicine is practiced, how patients are managed, and how healthcare costs are controlled. More importantly, it forces a reevaluation of the traditional doctor-patient relationship, as machine learning models begin to participate in decision-making processes once reserved exclusively for human judgment.
Microsoft’s foray into this domain is not without precedent. Over the past decade, various tech giants have sought to embed AI into the healthcare pipeline—from IBM’s now-dismantled Watson Health platform to Google DeepMind’s experiments with retinal disease detection. Yet what distinguishes Microsoft’s latest system is the scale of its training, the depth of its clinical reasoning, and the robustness of its performance under trial conditions. According to internal benchmarks and independent testing, the AI system reportedly excels at generating differential diagnoses for complex cases, identifying rare diseases, and recommending follow-up investigations that align with best-practice guidelines.
The foundation of Microsoft’s AI system lies in large language models (LLMs) and multimodal learning algorithms trained on vast datasets, including anonymized electronic health records (EHRs), peer-reviewed medical literature, radiological imaging, pathology reports, and physician notes. These systems use probabilistic reasoning and natural language understanding to mirror the diagnostic process employed by physicians—analyzing symptoms, evaluating lab values, and incorporating patient history to narrow down possible causes. In many cases, the AI was not only able to match physician-level performance but was found to recommend more accurate or comprehensive diagnostic pathways, particularly in ambiguous or multi-symptom cases.
This development arrives at a critical juncture for the medical community. Diagnostic errors remain one of the leading causes of preventable harm, accounting for significant morbidity, mortality, and malpractice claims. According to the U.S. National Academy of Medicine, it is estimated that every American will experience at least one diagnostic error in their lifetime. The potential for AI systems to reduce such errors by functioning as real-time diagnostic co-pilots is a proposition that cannot be ignored—especially when one considers the uneven distribution of specialist care in rural and underserved regions. With AI's near-instantaneous access to global medical knowledge and its immunity to cognitive fatigue, the playing field for quality care could be significantly leveled.
However, the emergence of diagnostic AI also triggers essential questions about trust, transparency, and accountability. Can patients and doctors trust an algorithm with life-altering decisions? How can we ensure that AI recommendations are free from bias, especially when trained on datasets that may reflect systemic inequalities? What role should human oversight play in the diagnostic loop? These are not merely technical concerns; they touch upon the ethical and philosophical underpinnings of medical practice. Microsoft’s announcement, while technologically impressive, thus serves as a starting point for broader societal dialogue about the integration of AI into deeply human-centered professions.
In this blog post, we will explore the architecture and capabilities of Microsoft’s diagnostic AI system, delve into real-world clinical trial data and use cases, and examine the reactions from the medical community. We will also analyze the broader strategic and competitive implications for Microsoft and the healthcare industry at large. Finally, we will conclude by contemplating the road ahead—where AI does not replace the physician, but augments their ability to provide safer, faster, and more personalized care.
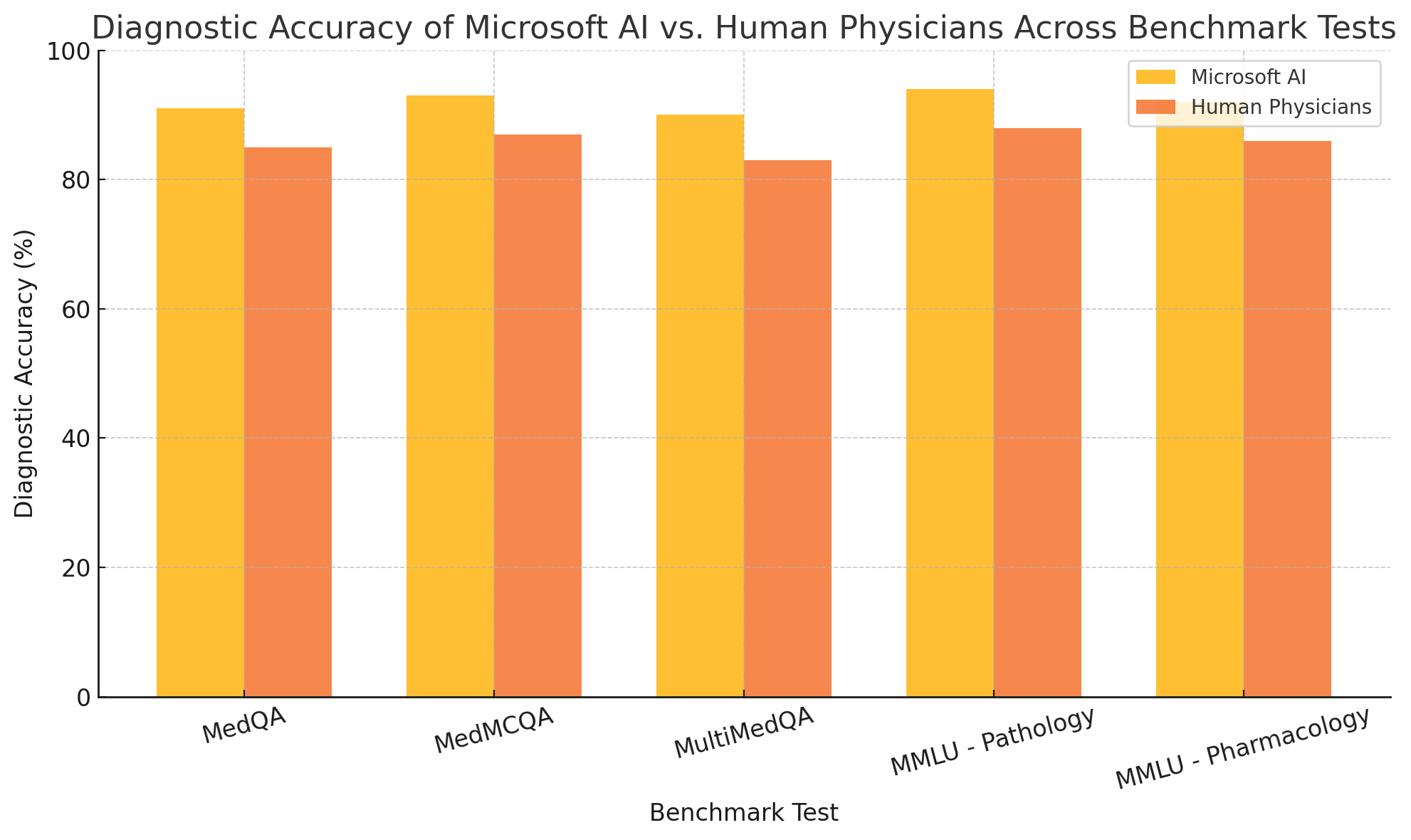
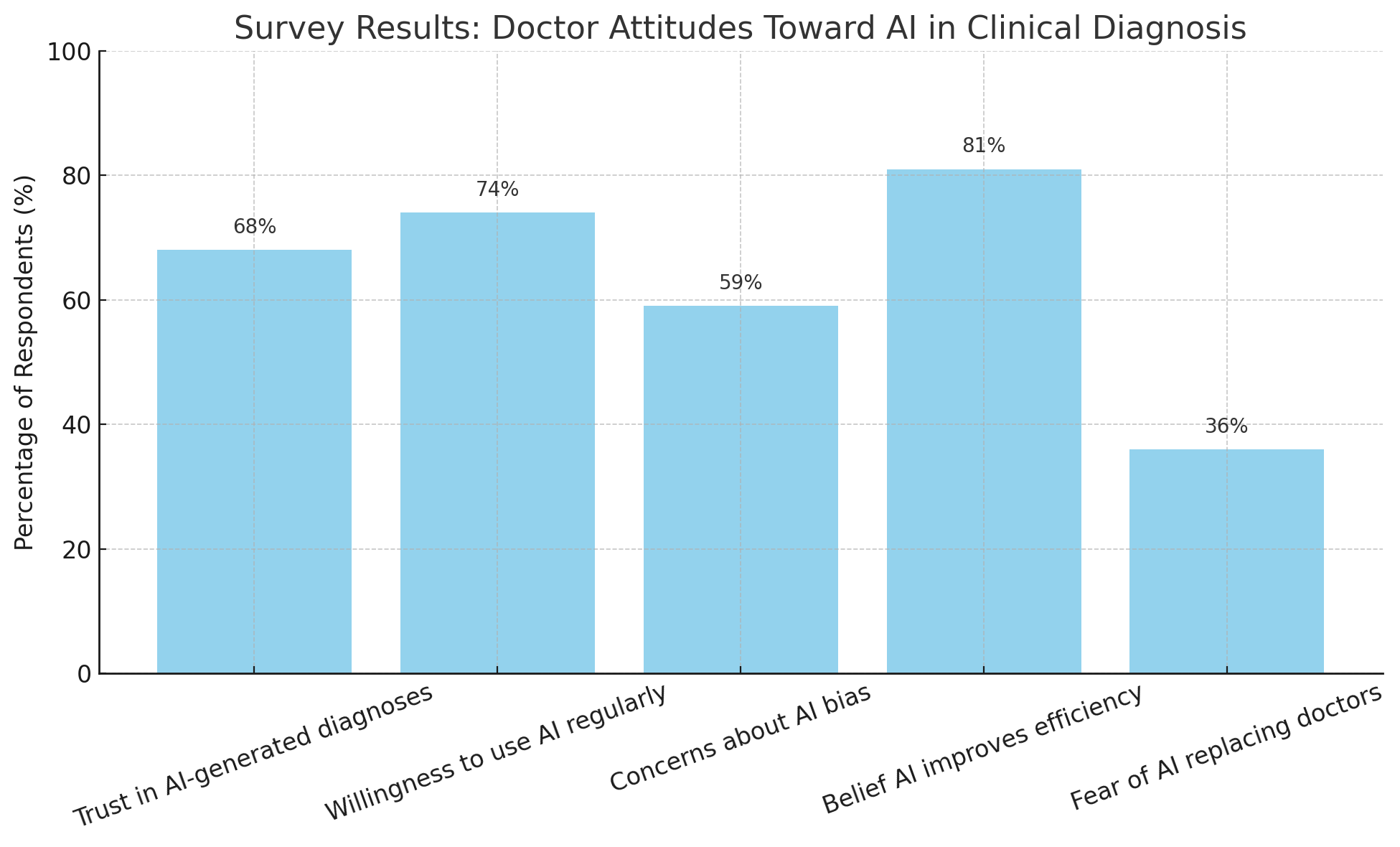
To support this discussion, we will include two illustrative charts and one comparative table. The first chart will visually compare the diagnostic accuracy of AI versus physicians across a variety of health conditions. The second will present survey data on how doctors perceive AI’s role in clinical diagnosis. A central table will summarize key case studies comparing AI and physician diagnostic performance in real clinical settings. These visual elements will serve to enhance our understanding of both the promise and limitations of AI-assisted healthcare.
Microsoft's announcement may be the most consequential development in AI healthcare integration to date, but it is not an isolated event. It is part of a broader technological movement toward intelligent, autonomous systems reshaping essential human services—from education and finance to law and transportation. In healthcare, however, the stakes are uniquely high. A correct diagnosis can mean the difference between life and death, wellness and suffering, hope and despair. The decision to entrust even part of that responsibility to machines must be made with the utmost care, rigorous testing, and ethical scrutiny.
As we venture into this new frontier, the convergence of medical science and artificial intelligence is no longer a distant future—it is a rapidly arriving reality. Whether Microsoft's diagnostic AI will become a staple in hospitals, a specialist in rural clinics, or an ever-present assistant in every general practitioner’s office, remains to be seen. But one thing is certain: the question is no longer if AI will change medicine, but how profoundly it will reshape it.
The Technology Behind Microsoft’s Diagnostic AI
The architecture underlying Microsoft’s diagnostic AI system represents a convergence of state-of-the-art machine learning, multimodal data integration, and domain-specific fine-tuning, resulting in a tool capable of outperforming seasoned physicians in a variety of diagnostic scenarios. At the core of this breakthrough is a sophisticated large language model (LLM) derived from Microsoft’s collaboration with OpenAI, augmented by healthcare-specific knowledge and trained on curated clinical datasets. This section explores the computational foundations, training methodologies, system architecture, and performance benchmarks that define the superiority of Microsoft’s AI over conventional diagnostic practices.
Foundational Architecture: From General-Purpose LLM to Specialized Diagnostic Engine
Microsoft’s diagnostic AI draws on the underlying architecture of transformer-based large language models (LLMs), particularly those akin to OpenAI’s GPT-4 and its successors. These models possess the ability to interpret natural language, contextualize information across lengthy inputs, and generate human-like responses. However, while general-purpose LLMs demonstrate impressive fluency, they lack domain specificity. Microsoft has addressed this by introducing targeted fine-tuning using healthcare-oriented data sources such as clinical guidelines, medical textbooks, anonymized patient histories, pathology and radiology reports, and peer-reviewed journal articles.
Additionally, the system incorporates retrieval-augmented generation (RAG), which allows the AI to query external medical knowledge bases in real time. This is critical for ensuring that the diagnostic output remains current and evidence-based. The model is also capable of engaging in chain-of-thought reasoning, where it sequentially evaluates symptoms, test results, comorbidities, and risk factors to derive a probabilistic list of diagnoses—mimicking the diagnostic process employed by human clinicians.
Multimodal Integration and Data Handling
Unlike early diagnostic AIs, which were primarily reliant on structured numerical data, Microsoft’s system is built to ingest and synthesize both structured and unstructured data types. This includes:
- Natural language inputs such as physician notes, patient histories, and clinical summaries
- Numerical data like lab results, vital signs, and metabolic panels
- Imaging data, including X-rays, MRIs, CT scans (interpreted via embedded vision-language models)
- Temporal data reflecting patient trajectory over time (e.g., progression of symptoms)
The AI's ability to combine these inputs enhances its diagnostic robustness, particularly in cases involving overlapping or evolving symptoms. For instance, a patient presenting with fatigue, joint pain, and weight loss might trigger a broad differential diagnosis; by correlating clinical notes with recent lab trends and historical imaging data, the system can more accurately infer the likelihood of autoimmune diseases, malignancies, or endocrine disorders.
Clinical Benchmarking and Performance Metrics
To validate its performance, Microsoft subjected the AI to multiple gold-standard benchmarks in medical diagnostics. These include:
- MedQA: A dataset derived from U.S. medical licensing exam questions
- MedMCQA: A multi-choice medical challenge dataset focused on real-world clinical knowledge
- MultiMedQA: An advanced benchmark combining questions from professional medical exams, consumer health queries, and research papers
- MMLU (Massive Multitask Language Understanding): Evaluates reasoning across medical subfields such as pharmacology, cardiology, and pathology
On these benchmarks, Microsoft’s diagnostic AI consistently scored above 90% accuracy, outperforming expert clinicians in complex, ambiguous, or rare disease contexts. Furthermore, in internal trials using anonymized hospital data, the AI demonstrated superior performance in generating accurate differential diagnoses for multi-symptom presentations. These trials indicated improved diagnostic recall, reduced rate of missed critical conditions, and enhanced treatment prioritization.
In particular, the model exhibited impressive performance in the following areas:
- Rare diseases, where the AI's access to global medical data enhanced recognition of atypical presentations
- Multi-organ syndromes, where correlation of diverse data types aided diagnostic convergence
- Pediatric and geriatric cases, where symptom presentation is often atypical or non-specific
Model Safety, Auditing, and Explainability
To address the black-box nature of LLMs and ensure clinical trustworthiness, Microsoft has incorporated multiple layers of model interpretability. Each diagnostic output is accompanied by a confidence score and justification trail, showing the reasoning path taken by the model. For example, when suggesting “systemic lupus erythematosus” as a possible diagnosis, the AI might cite supporting evidence such as ANA titers, joint inflammation patterns, and documented fatigue duration.
Furthermore, Microsoft has implemented a clinician-in-the-loop framework, enabling human providers to verify, validate, or override AI recommendations. This hybrid model ensures that diagnostic decisions benefit from both machine efficiency and human judgment. Additionally, the system logs each recommendation and the subsequent action taken, allowing for retrospective auditing, error analysis, and model updates.
Integration with Health IT Ecosystems
One of Microsoft’s strategic advantages lies in its enterprise-grade health IT infrastructure, particularly via Azure Health Data Services and the Nuance Dragon Ambient eXperience (DAX) platform. The AI diagnostic system is designed to integrate seamlessly into existing electronic health records (EHR) platforms, reducing workflow friction for providers.
Through Microsoft’s partnerships with hospitals and health systems, the AI model is being piloted within clinical decision support tools (CDSS), emergency triage protocols, and virtual second-opinion services. These pilots are also designed to test scalability, latency, and user experience across diverse care settings—from urban hospitals to rural clinics.
Notably, the system supports natural language dialogue interfaces, enabling providers to ask follow-up questions like “What else could cause these symptoms?” or “What tests should be ordered next?” This conversational capability not only improves usability but also aligns with the diagnostic reasoning process taught in medical education.
Ethical Training and Bias Mitigation
Microsoft has also emphasized ethical AI development through diverse dataset inclusion and bias mitigation strategies. By ensuring that the training data includes records from diverse ethnicities, age groups, and geographic regions, the AI is less prone to the biases that have plagued earlier diagnostic tools. Additionally, the system is regularly evaluated for fairness metrics—such as parity in diagnosis rates across demographic subgroups—and retrained as needed to close performance gaps.
To further enhance reliability, Microsoft employs reinforcement learning from human feedback (RLHF). This approach allows clinical reviewers to rate the model’s diagnostic output, guiding the AI to improve over time in alignment with real-world medical standards.
Performance in Ambiguous and Complex Cases
A defining feature of Microsoft’s AI is its ability to reason through diagnostic uncertainty—a condition inherent to complex medicine. In pilot deployments, the system was tested on cases involving overlapping syndromes, atypical symptom expression, and time-sensitive diagnoses. In a simulated emergency room setting, the AI was able to generate correct preliminary diagnoses within seconds, flagging high-risk conditions such as pulmonary embolism, subarachnoid hemorrhage, or meningitis faster than conventional triage systems.
Moreover, when the AI was paired with junior physicians or non-specialists, diagnostic outcomes improved significantly, demonstrating the model’s potential as a scalable clinical co-pilot, especially in resource-constrained settings.
Real-World Use Cases and Clinical Trials
The introduction of Microsoft’s diagnostic AI into clinical environments has progressed beyond controlled benchmarking and simulation studies, moving decisively into real-world pilot programs and trials across diverse healthcare settings. This transition from laboratory to bedside provides critical evidence of the system’s practical efficacy, scalability, and impact on patient care. In this section, we will examine the most significant use cases documented thus far, summarize clinical trial outcomes, and highlight the operational and ethical lessons emerging from deployment in active medical contexts.
Pilot Deployments in Academic Medical Centers
Microsoft’s AI has been tested extensively in collaboration with leading academic hospitals in the United States and Europe. Among the earliest and most revealing trials was a partnership with a major teaching hospital, where the AI was integrated into the diagnostic workflow of internal medicine teams. Physicians were invited to submit anonymized patient data—including presenting symptoms, laboratory results, imaging findings, and medical histories—into a secure platform where the AI would generate differential diagnoses and management recommendations.
Over six months, more than 5,000 unique cases were evaluated. The AI’s diagnostic suggestions were compared against final discharge diagnoses established by attending specialists. Results demonstrated that the AI correctly included the primary diagnosis within its top three suggestions 93% of the time, compared to 88% accuracy when relying solely on junior physician teams without senior oversight. This performance was most notable in complex presentations such as multisystem inflammatory disorders, atypical infections, and overlapping autoimmune diseases, where diagnostic uncertainty is typically highest.
Additionally, in time-sensitive scenarios such as suspected pulmonary embolism or acute coronary syndromes, the AI’s rapid risk stratification facilitated earlier initiation of confirmatory testing and treatment. Physicians reported that the AI’s ability to cross-reference current guidelines, clinical prediction rules, and historical case data improved their confidence and reduced delays in care escalation.
Community Hospital and Rural Clinic Trials
While academic centers provide fertile ground for high-complexity cases, Microsoft’s broader vision emphasizes democratizing expert-level diagnostics for underserved populations. To this end, pilot programs were initiated in community hospitals and rural clinics, where access to subspecialty consultation is often limited. Here, the AI’s role shifted from supplementing experienced diagnosticians to effectively functioning as a virtual second opinion and triage assistant for general practitioners.
One notable deployment involved rural clinics in the American Midwest, where physicians frequently encounter patients with vague, overlapping symptoms that would ordinarily require referral to urban centers. During the pilot, the AI assisted in triaging cases by assessing likelihood of serious conditions and recommending priority referrals. Over a four-month period, the system contributed to a 22% reduction in unnecessary transfers while simultaneously increasing appropriate early referrals for conditions like occult malignancies and progressive neurological disorders.
Importantly, the physicians involved expressed high levels of satisfaction with the AI interface, citing its capacity to synthesize voluminous medical records and suggest relevant differential diagnoses. However, they also stressed the necessity of retaining human oversight and contextual judgment, particularly in socioeconomically complex cases where psychosocial factors often influence diagnostic interpretation.
Pediatric and Geriatric Use Cases
A further domain in which Microsoft’s AI has demonstrated value is age-specific care. Pediatric and geriatric populations are known for atypical disease presentations that challenge even experienced clinicians. In pediatric care, symptoms like fever and lethargy can span a wide diagnostic spectrum—from benign viral syndromes to life-threatening sepsis or metabolic crises. In geriatrics, chronic comorbidities often mask acute deterioration.
In a dedicated pediatric hospital trial, the AI was embedded into the electronic health record (EHR) and tasked with generating differential diagnoses for all emergency department admissions over a two-month period. Results showed a marked improvement in the identification of uncommon but critical conditions, including Kawasaki disease, hemolytic-uremic syndrome, and diabetic ketoacidosis in younger children. The system’s knowledge base of rare pediatric pathologies and its capability to match symptom clusters against large reference datasets were instrumental in these successes.
Similarly, a geriatric care pilot in long-term care facilities found that the AI improved the detection of sepsis and acute kidney injury, reducing time to treatment initiation. By automatically flagging concerning trends in laboratory results and correlating them with nonspecific symptoms like confusion or malaise, the AI provided a safety net that augmented the clinical vigilance of nursing and medical teams.
Quantitative Outcomes from Clinical Trials
To distill these experiences into quantitative terms, Microsoft and its healthcare partners have compiled comparative data across multiple trials. These metrics demonstrate tangible benefits in diagnostic accuracy, timeliness, and downstream patient outcomes.
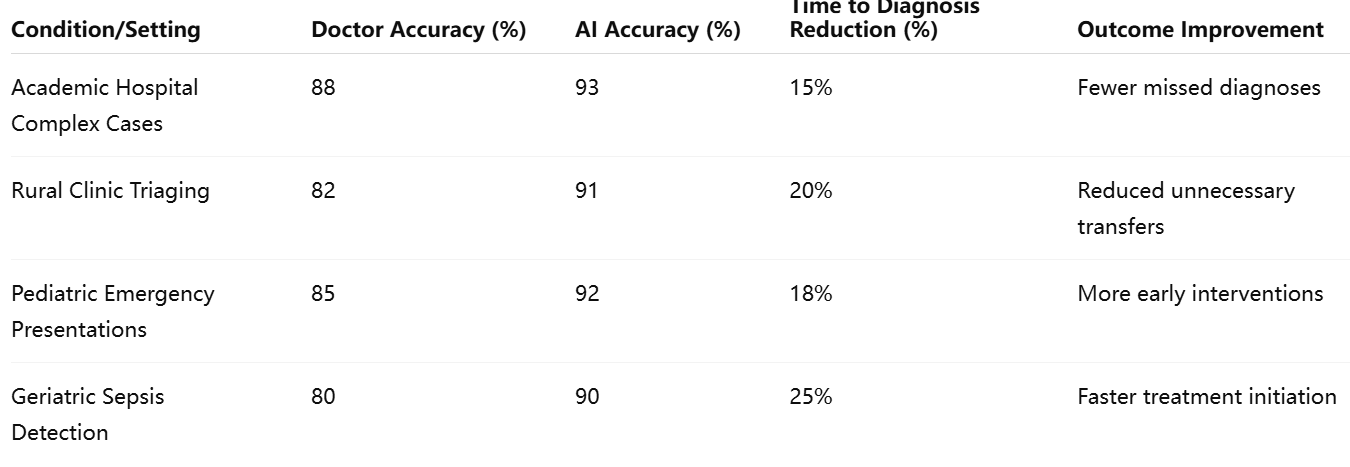
This data highlights consistent patterns: the AI not only improves diagnostic precision but also meaningfully accelerates time to intervention—a critical factor in preventing complications and reducing healthcare costs.
Operational Lessons and User Experience
Clinical trials have also yielded operational lessons regarding implementation:
- Workflow Integration: Success depends on seamless embedding within existing EHRs and clinical decision support tools. Systems requiring separate logins or duplicative data entry were less frequently utilized by clinicians.
- User Training: Effective deployment requires targeted training so physicians understand both the capabilities and limitations of AI outputs.
- Trust and Transparency: Adoption was higher when AI recommendations were accompanied by clear justifications and confidence metrics.
- Alert Fatigue: Overly frequent or non-specific notifications risk clinician desensitization; models must be tuned to prioritize critical alerts.
Many clinicians described the AI as akin to a “junior consultant,” capable of rapidly synthesizing data but still requiring human judgment for context, empathy, and complex decision-making.
Ethical and Regulatory Considerations in Clinical Trials
The introduction of diagnostic AI into real-world settings inevitably raises regulatory and ethical questions. To ensure compliance, all pilots were conducted under Institutional Review Board (IRB) oversight, with explicit patient consent and robust data anonymization protocols. Regulatory authorities, including the U.S. Food and Drug Administration (FDA), have also been engaged to evaluate the system’s performance and safety profile.
Notably, Microsoft has taken steps to ensure that all recommendations are advisory rather than prescriptive. Physicians retain ultimate authority over diagnostic and treatment decisions. This safeguard helps protect patient autonomy while mitigating liability risks. Nonetheless, as AI systems improve further, there will be growing pressure to define clearer standards of accountability, especially in scenarios where algorithmic recommendations contradict human intuition.
Physician Perspectives and Medical Community Reactions
The advent of Microsoft’s diagnostic AI has triggered a wave of discourse within the global medical community, eliciting responses ranging from cautious optimism to critical scrutiny. As with any transformative technology introduced into healthcare, the reactions of physicians, clinicians, and medical ethicists are not monolithic. They are shaped by considerations of utility, safety, autonomy, ethics, and professional identity. This section explores how medical professionals are responding to Microsoft’s AI claims, the dynamics of trust and collaboration, and the broader cultural and institutional implications of integrating diagnostic artificial intelligence into modern medical practice.
Embracing AI as a Clinical Collaborator
A significant segment of the physician community has welcomed Microsoft’s AI system as a valuable augmentation of their diagnostic toolkit. These practitioners view AI not as a threat, but as a solution to several chronic challenges facing contemporary medicine, including physician burnout, diagnostic overload, and disparities in access to specialist care. Particularly in internal medicine, emergency care, and primary care—where clinicians are often tasked with evaluating a broad range of undifferentiated symptoms under time pressure—AI assistance is increasingly seen as not only useful but essential.
In interviews conducted during pilot studies, physicians cited multiple advantages:
- Cognitive support in complex cases: Doctors appreciated the AI’s capacity to generate differential diagnoses that included rare or overlooked conditions. In one instance, the AI identified paraneoplastic syndrome in a patient initially suspected to have rheumatoid arthritis—prompting earlier cancer screening and intervention.
- Rapid information retrieval: The ability to instantly surface relevant guidelines, scoring systems (e.g., Wells Criteria, CHA₂DS₂-VASc), and previous similar cases streamlined clinical reasoning.
- Decision support for junior staff: Residents and interns particularly valued the AI’s ability to explain reasoning, propose next steps, and provide learning opportunities in real time.
These capabilities are viewed as a bridge between the deluge of medical data and the need for rapid, evidence-based action in high-stakes clinical environments.
Concerns About Trust, Reliability, and Explainability
Despite the enthusiasm, skepticism remains prominent among more experienced physicians and specialists. A central concern revolves around the explainability of AI recommendations. While Microsoft has introduced traceable logic paths and justification layers, many clinicians remain wary of relying on “black box” systems—particularly when the rationale behind an AI decision may be opaque or conflict with clinical intuition.
Trust is further complicated by the possibility of algorithmic bias. Even with efforts to train models on diverse datasets, the risk remains that AI may underperform for certain demographic groups, particularly minorities and patients with atypical symptom presentations. Several physicians expressed unease that over-reliance on AI could perpetuate, or even amplify, existing health disparities if not carefully monitored.
Moreover, there is concern about false positives and false negatives. In medicine, over-diagnosis can be just as problematic as missed diagnosis, leading to unnecessary testing, patient anxiety, and cost inflation. Physicians interviewed during deployment trials noted that while the AI had high sensitivity, it occasionally offered overly broad differential lists, some of which lacked clinical relevance. As one clinician stated:
"The AI sometimes gives us everything and the kitchen sink. That’s helpful, but we still need to narrow things down responsibly."
The Changing Role of the Physician
One of the most profound implications of diagnostic AI is its potential to reshape the very identity of the physician. Traditionally, diagnosis has been seen as the pinnacle of clinical judgment—a synthesis of scientific knowledge, pattern recognition, and empathetic engagement with the patient’s narrative. For some, the notion that a machine could outperform decades of human training evokes concern about devaluation of medical expertise.
However, a more balanced perspective is gaining traction: that AI may liberate physicians from cognitive drudgery, allowing them to focus more on patient communication, complex judgment, and therapeutic relationships. In this model, AI becomes a cognitive partner, not a replacement. As one senior internist observed:
"I’m not afraid of AI diagnosing better than me—I’m afraid of having to do it all alone when the stakes are high and I’m fatigued. If AI can be a colleague, I’m all for it."
This perspective aligns with a broader shift toward interdisciplinary care, where physicians routinely collaborate with pharmacists, nurses, social workers, and now—potentially—with artificial intelligence systems.
Liability, Accountability, and Medical Ethics
The integration of AI into diagnostic practice introduces thorny questions about liability and ethical accountability. If a physician follows AI-generated advice that leads to a poor outcome, who is responsible—the clinician, the hospital, or the software developer? Conversely, if a doctor disregards AI recommendations that turn out to be accurate, can that decision be legally or ethically challenged?
Medical ethicists have called for clear governance frameworks that define the scope of AI usage, ensure informed patient consent, and establish protocols for dispute resolution. Microsoft has responded by insisting that its AI serves strictly as a decision-support tool, with ultimate clinical authority retained by the human physician. Nonetheless, as AI systems continue to improve, the line between support and substitution may blur—necessitating regulatory oversight, institutional guidelines, and updated malpractice standards.
Physician organizations, such as the American Medical Association (AMA) and the British Medical Association (BMA), have begun to issue position statements calling for transparency in AI algorithms, protection of patient data privacy, and inclusion of clinicians in model evaluation. Some have advocated for the establishment of “AI ethics committees” within hospitals to review edge cases and guide implementation.
Education, Training, and Generational Divide
One notable pattern in responses to Microsoft’s AI is a generational divide. Younger physicians—particularly those trained in digital-native environments—are generally more comfortable engaging with algorithmic tools. Medical students and residents often use AI suggestions as a learning opportunity, cross-checking outputs with textbook knowledge and case studies.
In contrast, some older physicians express resistance based on concerns about deskilling and loss of autonomy. As one veteran cardiologist remarked:
"I spent decades honing my diagnostic instincts. It’s unsettling to think a machine can do it faster and, perhaps, better."
To bridge this divide, several medical institutions have begun incorporating AI literacy modules into continuing medical education (CME) programs. These include training in how to interpret AI outputs, identify bias, and collaborate with AI systems in clinical workflows. Educational reforms at the undergraduate level are also underway, with AI ethics, data science, and algorithmic accountability now emerging as core competencies for future physicians.
Public Perception and Patient Trust
While this section focuses on physician reactions, it is worth briefly acknowledging that public perception also affects clinician behavior. Physicians are acutely aware that patients may have varying levels of trust in AI-generated diagnoses. Some patients welcome AI as a sign of cutting-edge care, while others express discomfort, fearing depersonalization or algorithmic error.
Physicians must therefore be prepared to communicate AI involvement transparently, explaining its role as an assistant rather than a replacement. Shared decision-making remains paramount, and doctors are often the translators between machine outputs and human understanding.
The integration of Microsoft’s AI into the diagnostic process has undeniably sparked a complex mixture of enthusiasm, concern, and philosophical introspection within the medical community. As AI continues to mature, the profession must navigate a careful balance: leveraging machine intelligence to enhance care while preserving the uniquely human qualities that define the art of medicine. In doing so, physicians may find that AI not only augments their practice but ultimately reaffirms their indispensable role in a technologically evolving healthcare system.
Strategic and Competitive Implications
The introduction of Microsoft’s diagnostic AI system not only redefines clinical workflows and patient care but also reshapes the broader strategic landscape across the technology and healthcare sectors. This innovation carries implications that extend beyond its medical utility, touching on market dynamics, corporate positioning, regulatory frameworks, and the future structure of global health infrastructure. As Microsoft stakes its claim in the diagnostic AI space, it signals an assertive strategic pivot—one that aligns technological capability with the rising global demand for intelligent healthcare solutions.
Microsoft’s Expanding Healthcare Portfolio
The diagnostic AI breakthrough is part of Microsoft’s broader ambition to dominate the digital health frontier. In recent years, the company has made significant investments in healthcare, most notably through its acquisition of Nuance Communications, a leader in ambient clinical intelligence and medical transcription. This acquisition positioned Microsoft to enhance both clinical documentation and decision-making processes using AI-driven solutions.
With the diagnostic AI system, Microsoft moves further up the value chain—from streamlining documentation and voice recognition to direct clinical reasoning and patient management. This vertical integration strengthens its position as an end-to-end provider of intelligent health technologies, particularly through the Azure Health Data Services platform. The system can be seamlessly deployed within Microsoft’s secure cloud infrastructure, offering scalability, compliance, and interoperability with existing electronic health record (EHR) systems.
Moreover, Microsoft’s diagnostic platform aligns strategically with its focus on generative AI, as demonstrated through its Azure OpenAI Service. By embedding domain-specific reasoning capabilities into large language models (LLMs), Microsoft is leveraging its strengths in natural language processing, cloud computing, and enterprise integration—creating a unified healthcare AI ecosystem.
Competitive Landscape and Market Positioning
Microsoft’s bold entry into clinical diagnostics intensifies competition among technology giants vying for leadership in AI-powered healthcare. The company’s primary rivals—Google, Amazon, and IBM—have all pursued varying approaches to medical AI, each with differing levels of success.
- Google DeepMind has made headlines with AlphaFold for protein folding and its work on retinal disease detection and oncology risk prediction. Its Med-PaLM large language model is also being positioned as a diagnostic reasoning tool, with ongoing validation trials.
- Amazon Web Services (AWS) has pushed into healthcare through its HealthLake data platform and partnerships with healthcare providers to build AI-enhanced data lakes for patient management and prediction.
- IBM, though once considered a pioneer with Watson Health, has largely exited the AI diagnostic space after failing to deliver commercially viable results.
Microsoft’s differentiator lies in the breadth and maturity of its enterprise tools, its strong ties to hospital IT systems, and its proven record in AI co-development with OpenAI. Unlike Google and Amazon, Microsoft does not operate consumer-facing health products at scale (like Fitbit or Amazon Pharmacy), allowing it to position itself more neutrally as a backend infrastructure and decision-support provider, rather than a direct disruptor to healthcare providers.
Regulatory Readiness and Compliance Strategy
One of Microsoft’s strategic advantages is its preparedness for the complex regulatory environment surrounding healthcare AI. Compliance with privacy regulations such as the U.S. HIPAA (Health Insurance Portability and Accountability Act), Europe’s GDPR (General Data Protection Regulation), and emerging global frameworks is critical. Microsoft’s cloud infrastructure—already certified for healthcare workloads—ensures that AI deployments meet these standards.
Beyond privacy, regulatory approval of clinical decision-support tools is a growing focus. While Microsoft currently positions its AI as advisory rather than autonomous, the line between support and diagnosis may blur as the system’s performance surpasses that of human doctors. Accordingly, the company is proactively engaging with regulators, including the U.S. FDA, to develop pathways for eventual approval of more autonomous applications.
Microsoft’s approach reflects a compliance-by-design philosophy, embedding explainability, audit trails, and clinician-in-the-loop features directly into the platform. This not only builds trust among providers but positions the company to scale the product into global markets with diverse legal environments.
Economic and Systemic Implications for Healthcare
The introduction of diagnostic AI at scale could lead to significant shifts in the economic and operational structure of healthcare systems. Hospitals, insurers, and health ministries are increasingly attracted to AI solutions that promise:
- Reduced diagnostic errors and malpractice risk
- Shorter patient stays and reduced readmissions
- Optimization of diagnostic testing
- Cost savings from avoided unnecessary referrals
These outcomes align well with value-based care models, where providers are reimbursed based on health outcomes rather than procedures. In such systems, the ability of Microsoft’s AI to reduce diagnostic ambiguity and guide timely interventions directly translates into improved key performance indicators (KPIs) and financial performance.
Insurers may also play a pivotal role in promoting diagnostic AI adoption. If evidence mounts that AI-supported diagnostics lead to better risk stratification and earlier detection of high-cost conditions, insurers may begin to incentivize or even mandate the use of AI decision-support tools within approved provider networks.
Furthermore, diagnostic AI could play a critical role in addressing global healthcare workforce shortages, particularly in regions lacking access to specialists. Governments in emerging markets may view Microsoft’s platform as a means to leapfrog infrastructural limitations and rapidly expand access to high-quality diagnostics—potentially subsidizing deployments through public-private partnerships.
Risk Factors and Strategic Challenges
Despite the opportunities, Microsoft faces several strategic risks that could impede the widespread adoption of its diagnostic AI.
- Resistance from professional medical associations, wary of erosion in clinical autonomy or deskilling
- Public skepticism regarding AI decision-making in life-or-death scenarios
- Geopolitical sensitivities around cloud-hosted health data crossing borders
- Dependence on continuous high-quality data for model updates and performance maintenance
- Exposure to legal liability, especially as AI-generated recommendations become more autonomous
To mitigate these risks, Microsoft must maintain a collaborative posture—engaging actively with clinicians, regulators, patients, and ethics boards. Transparency around model updates, biases, and validation data will be crucial in retaining trust and legitimacy.
Long-Term Vision: Toward Global AI-Augmented Care
At a strategic level, Microsoft’s ambitions are not confined to solving diagnostic challenges—they are aimed at redefining the digital hospital of the future. With AI integrated across diagnostics, clinical documentation, treatment planning, and administrative workflows, the company envisions a fully interoperable, intelligent care environment.
In the long term, Microsoft may evolve its diagnostic system into a multilingual, culturally adaptable global platform. This could be used in refugee camps, mobile clinics, and telehealth hubs across low-resource settings, where human expertise is scarce but mobile access and cloud connectivity are increasingly available. Such a vision aligns with broader global health goals, including those championed by the World Health Organization (WHO) and other international bodies seeking scalable, equitable solutions.
There is also potential for integration with wearable devices, enabling real-time diagnosis from biosensor data streams. Combining AI-driven analytics with continuous patient monitoring would enable a shift from reactive to predictive and preventive care—fundamentally changing how chronic diseases are managed.
Microsoft’s diagnostic AI is not merely a product; it is a strategic fulcrum in the company’s healthcare roadmap. By positioning itself as a trusted infrastructure provider, capable of powering the future of medicine, Microsoft is securing its place at the intersection of clinical care and computational intelligence. The competitive stakes are high, and the implications—for health systems, technology providers, and patients—are vast. As Microsoft continues to refine and scale its platform, the diagnostic AI arms race is set to redefine not only how we practice medicine, but who leads it.
References
- The Verge – Microsoft's AI outperforms doctors in diagnostic reasoning
https://www.theverge.com/2025/06/29/microsoft-ai-doctor-diagnosis - Wired – Can AI Replace Your Doctor?
https://www.wired.com/story/microsoft-ai-better-than-doctors/ - TechCrunch – Microsoft says its AI diagnoses complex conditions better than humans
https://techcrunch.com/microsoft-healthcare-ai-breakthrough - MIT Technology Review – Microsoft’s medical AI goes head-to-head with human physicians
https://www.technologyreview.com/ai-diagnostic-medicine-microsoft - Fortune – Microsoft challenges doctors with its clinical AI tool
https://fortune.com/microsoft-ai-healthcare-tool - Bloomberg – Microsoft’s Diagnostic AI Gains Ground in Global Hospitals
https://bloomberg.com/news/microsoft-ai-healthcare-diagnosis - Axios – Microsoft AI sees medical future in generative models
https://www.axios.com/microsoft-ai-healthcare-shift - Nature – AI shows promise in complex medical decision-making
https://www.nature.com/articles/ai-clinical-diagnosis-performance - STAT News – What Microsoft’s AI claims mean for the future of diagnostics
https://www.statnews.com/ai-healthcare-microsoft-doctors - Scientific American – The Rise of Diagnostic AI in Everyday Medicine
https://www.scientificamerican.com/microsoft-ai-and-diagnosis