AI Forecasting Revolutionizes Diabetes Care: Inside IBM and Roche’s Predictive Health Partnership

Diabetes remains one of the most pervasive chronic diseases worldwide, affecting over half a billion people and accounting for immense human and economic costs. As of recent estimates, more than 1 in 10 adults globally live with diabetes, with the figure projected to rise significantly over the next decade. While both Type 1 and Type 2 diabetes present distinct clinical challenges, they share a common requirement: the precise management of blood glucose levels. This task, though foundational to patient health, remains fraught with difficulty, uncertainty, and often, inconsistency.
The core challenge lies in the dynamic nature of glucose levels, which fluctuate based on diet, activity, stress, medication adherence, illness, and even sleep. Despite advancements in continuous glucose monitors (CGMs) and insulin delivery systems, a majority of patients still struggle to maintain optimal glycemic control. This leads to frequent episodes of hypoglycemia (low blood sugar) or hyperglycemia (high blood sugar), both of which can result in serious long-term complications such as cardiovascular disease, kidney failure, vision loss, and nerve damage.
Conventional diabetes management approaches—while clinically sound—are reactive in nature. Patients are often required to monitor their glucose levels multiple times a day and manually respond to fluctuations. Even with the use of modern CGMs, users must interpret the data and make critical decisions in real time. Such processes place a significant cognitive and emotional burden on individuals managing the condition daily. In this context, the integration of artificial intelligence (AI) emerges as a transformative solution capable of predicting, rather than merely reporting, blood sugar fluctuations.
Artificial intelligence offers the potential to revolutionize chronic disease management by moving healthcare from a reactive to a predictive paradigm. Leveraging large-scale data, machine learning algorithms can identify subtle patterns and trends in blood glucose data, combined with behavioral, physiological, and contextual inputs. When properly trained and validated, these systems can forecast future glycemic events and provide actionable insights, allowing patients and providers to intervene proactively rather than retroactively.
It is within this technological frontier that global leaders IBM and Roche have forged a strategic collaboration aimed at tackling diabetes through AI-driven forecasting. Roche, a leading pharmaceutical and diagnostics firm with deep expertise in diabetes care, brings its Accu-Chek portfolio and vast clinical data resources. IBM, a global technology company known for pioneering AI through its Watson platform, contributes its machine learning infrastructure, cloud computing capabilities, and healthcare domain knowledge. Together, they aim to develop intelligent systems capable of real-time and personalized blood glucose predictions for individuals managing diabetes.
This collaboration represents more than a technological partnership; it reflects a broader shift in the healthcare ecosystem toward precision medicine, where interventions are tailored to each patient’s unique profile and circumstances. The joint effort by IBM and Roche signals a future where data is not only collected and visualized but interpreted, contextualized, and transformed into timely, individualized recommendations.
This blog post will explore the inner workings and strategic impact of IBM and Roche’s AI initiative in diabetes management. It will examine the technical underpinnings of the AI model, its integration into daily care routines, and its implications for clinical outcomes. It will also discuss the potential challenges surrounding data privacy, ethical considerations, and the evolving role of healthcare professionals in an AI-augmented world.
As AI continues to mature and embed itself across sectors, its promise in healthcare—and specifically in diabetes—presents one of the most compelling cases for its transformative power. By forecasting blood sugar levels before they become problematic, this new generation of AI-powered tools could drastically improve quality of life, reduce emergency incidents, and pave the way for a new era in chronic disease care.
The AI Approach: How IBM and Roche Forecast Blood Glucose Trends
The application of artificial intelligence in diabetes management hinges on the capacity to analyze massive volumes of data in real time, learn from historical trends, and deliver predictive insights tailored to individual users. In the case of IBM and Roche’s joint venture, this capability has been refined into a sophisticated AI-driven system designed to forecast blood glucose fluctuations before they become medically significant. This section explores the technical framework, data architecture, and integration mechanisms that power this intelligent forecasting platform.
At the core of the system is a robust machine learning model trained on multi-dimensional datasets. These datasets include continuous glucose monitoring (CGM) outputs, insulin dosage records, nutritional inputs, physical activity levels, sleep patterns, stress indicators, and other contextual parameters collected from wearable devices and patient-reported data. The model architecture leverages both supervised and unsupervised learning algorithms to detect non-linear patterns and anticipate glycemic variability.
IBM’s contribution to the initiative centers on the deployment of advanced AI models using its Watson Health platform, now integrated into a broader AI and data services portfolio. These models are hosted on a secure, scalable cloud infrastructure that enables rapid data ingestion, preprocessing, and inferencing. The system applies recurrent neural networks (RNNs), particularly long short-term memory (LSTM) architectures, which are well-suited for time-series data like blood glucose readings. By analyzing historical input-output sequences, the LSTM models can forecast glucose levels up to several hours into the future with clinically relevant accuracy.
In parallel, Roche contributes its domain-specific expertise through devices such as the Accu-Chek line of glucose meters and insulin delivery systems, as well as through access to anonymized patient data acquired through decades of clinical practice and research. This data serves as a critical component for training and validating the machine learning models. Furthermore, Roche ensures that the AI recommendations are medically sound, aligning with established guidelines in endocrinology and diabetes management.
The forecasting system functions by continuously synchronizing with a patient’s CGM device or smart insulin pen. Upon data ingestion, the AI engine normalizes and analyzes the data stream, accounting for external variables such as meals, physical exertion, and emotional stress. For instance, a spike in blood glucose levels detected after a carbohydrate-rich meal may be projected to return to baseline within a specific timeframe, provided there is evidence of insulin administration and anticipated physical activity.
In practice, this system allows the generation of highly individualized forecasts. A user may receive a notification stating that their blood sugar is projected to fall below 70 mg/dL in the next 90 minutes, prompting them to consume fast-acting carbohydrates or adjust their insulin dosing. In more advanced configurations, the system could integrate with automated insulin delivery platforms, allowing for real-time, autonomous adjustments without requiring direct patient intervention—a step toward the long-envisioned “artificial pancreas.”
A critical advantage of this AI approach is the incorporation of adaptive learning mechanisms. Unlike static models, IBM and Roche’s forecasting engine evolves over time based on a patient’s unique physiological responses and behavior patterns. For example, if a patient’s insulin sensitivity changes due to weight loss or medication adjustments, the AI system adapts accordingly, refining its predictive outputs to maintain accuracy and clinical relevance.
Explainability, a common concern in AI healthcare applications, is addressed through model interpretability frameworks. IBM has integrated explainable AI (XAI) techniques into the system, ensuring that both patients and clinicians can understand the rationale behind a prediction. Instead of simply issuing a numerical forecast, the system provides contextual explanations, such as “Glucose predicted to rise due to recent high-carb meal and no insulin detected.” This transparency builds trust, improves adherence, and facilitates shared decision-making between patients and providers.
Furthermore, the user interface—whether accessed through Roche’s diabetes management apps or integrated platforms—is designed for clarity and accessibility. Visual dashboards display glucose trends, projected trajectories, and actionable recommendations in an intuitive manner. Users can also access retrospective analyses to understand how past decisions influenced glucose variability, creating a feedback loop for continuous learning and behavioral improvement.
The infrastructure supporting this system is fortified with security and compliance protocols that align with international standards, including HIPAA (Health Insurance Portability and Accountability Act) in the United States and GDPR (General Data Protection Regulation) in the European Union. All personal health information (PHI) is encrypted, and user consent protocols are rigorously applied. Moreover, IBM and Roche have implemented federated learning options for future iterations, allowing model training to occur locally on user devices, minimizing data transmission and enhancing privacy.
Interoperability is another focal point of the AI framework. The system is designed to interface seamlessly with electronic health records (EHRs), telehealth platforms, and third-party health applications. This integration enables clinicians to access patient data in context and align AI-driven forecasts with broader treatment plans. For healthcare providers managing large patient cohorts, the forecasting system can also assist in risk stratification, identifying individuals who may require proactive intervention.
One of the most innovative elements of the IBM-Roche platform is its capacity to simulate counterfactual scenarios. By adjusting input variables—such as removing a meal or modifying insulin timing—the AI engine can generate alternative glucose trajectories. This feature enables patients to explore the impact of different choices, fostering education and engagement. It also provides clinicians with tools to test hypothetical interventions before making adjustments to a care plan.
Importantly, the system is designed with scalability in mind. It can accommodate a wide range of users, from newly diagnosed patients with limited data history to advanced users managing complex regimens. Localization options are being developed to support multiple languages and region-specific dietary patterns, ensuring the system is inclusive and globally deployable.
Taken together, the AI forecasting model developed by IBM and Roche represents a significant advancement in diabetes care. By combining real-time monitoring, predictive analytics, and user-centric design, it addresses long-standing gaps in glycemic management and empowers individuals with actionable insights. This not only improves clinical outcomes but also enhances the quality of life for millions living with diabetes.
Clinical and Consumer Benefits: Personalization, Safety, and Outcomes
The integration of artificial intelligence into diabetes management, as demonstrated by the IBM and Roche collaboration, delivers a range of tangible benefits that extend across both clinical settings and personal health contexts. By enabling precise blood glucose forecasting, this AI-enhanced system transforms how patients manage their condition daily while equipping healthcare providers with actionable insights to optimize long-term care. This section explores the multifaceted value of AI-powered diabetes tools, with particular emphasis on personalization, safety, and clinical outcomes.
One of the most revolutionary advantages of AI in diabetes care is its capacity for personalization. Traditional monitoring approaches—such as manual blood glucose logging or basic continuous glucose monitoring—offer valuable data, but they often fail to translate that data into individualized predictions or recommendations. The forecasting system developed by IBM and Roche bridges this gap by tailoring insights to each patient’s physiological, behavioral, and lifestyle profile. This is made possible by the AI model’s ability to learn from longitudinal data, refining its predictions based on a patient’s unique glycemic responses to specific meals, physical activity levels, insulin regimens, stress events, and even sleep patterns.
This highly individualized approach has profound implications for glycemic control. By predicting glucose excursions in advance, patients can take proactive steps—such as adjusting meal timing, modifying insulin doses, or planning physical activity—to maintain their glucose levels within the recommended range. This reduces the frequency and severity of both hyperglycemic and hypoglycemic episodes, which are among the leading causes of emergency hospital visits for individuals with diabetes. Maintaining tighter glucose control is also correlated with a significant reduction in long-term complications, including cardiovascular disease, neuropathy, nephropathy, and retinopathy.
Furthermore, the AI system enhances safety, especially in high-risk situations. For patients with Type 1 diabetes, nocturnal hypoglycemia poses a particularly grave threat due to the absence of conscious monitoring during sleep. AI-driven forecasting systems can identify early warning signs and alert users or caregivers before a dangerous drop in blood sugar occurs. In advanced implementations, the system may also interface with insulin pumps or automated insulin delivery (AID) platforms, triggering preventive adjustments in basal insulin rates without the need for user intervention. This “closed-loop” functionality represents a major advancement toward achieving the goal of an artificial pancreas—a system that can independently regulate glucose levels in real time.
Another critical benefit of the AI-powered forecasting system is its support for patient education and engagement. The explainability mechanisms embedded in the IBM-Roche model do not merely provide numerical forecasts; they offer contextual explanations that help users understand the why behind each prediction. For instance, if a patient’s blood glucose is forecasted to spike, the system may cite a missed insulin dose following a carbohydrate-rich meal. This type of feedback fosters a deeper understanding of one’s condition and reinforces learning through real-world consequences, ultimately encouraging greater self-efficacy.
Patient feedback from early deployments and pilot studies underscores this point. Many users report feeling more confident and less anxious in their daily diabetes management routines when assisted by predictive AI tools. The ability to anticipate issues rather than constantly react to them shifts the patient’s role from passive responder to empowered decision-maker. In particular, newly diagnosed individuals and pediatric patients—groups that often experience emotional and cognitive burdens in managing diabetes—stand to benefit significantly from intuitive, AI-enhanced systems that support rather than overwhelm.
The benefits extend equally to clinicians and diabetes educators. In a conventional care model, healthcare professionals often rely on limited datasets—such as periodic glucose logs or HbA1c scores—to assess a patient’s condition. This snapshot view fails to capture the full spectrum of daily variability and behavioral factors that influence glycemic control. AI-driven forecasting tools provide a continuous, dynamic profile of patient data, complete with risk indicators and predictive trajectories. As a result, clinicians can make more informed decisions during consultations and tailor treatment plans with greater precision.
Moreover, the integration of the AI system with electronic health records (EHRs) and clinical dashboards allows for population-level analysis and proactive care planning. For instance, providers can identify patients who are at increased risk of glycemic instability and prioritize them for intervention. This is particularly valuable in resource-constrained settings, where clinical time and attention must be strategically allocated. It also supports emerging models of care, such as remote patient monitoring (RPM) and virtual diabetes clinics, where digital tools play a central role in maintaining continuity of care outside traditional clinical environments.
From a health economics perspective, AI-powered forecasting has the potential to significantly reduce healthcare costs associated with diabetes. By preventing severe hypoglycemic events, reducing hospital admissions, and delaying the onset of long-term complications, these systems can lower the financial burden on healthcare systems and insurers. According to various estimates, improved glycemic control through digital intervention could lead to cost savings in the billions annually when scaled across national healthcare programs.
A compelling illustration of the benefits can be found in comparative outcome studies and case analyses. Users who adopt AI-assisted monitoring show marked improvements across key clinical indicators. These include increased “time in range” (the percentage of time a patient’s glucose levels remain within target thresholds), decreased glucose variability (a key predictor of complications), and fewer emergency interventions. Improvements are often visible within weeks of implementation, particularly among patients who previously struggled with inconsistent management.
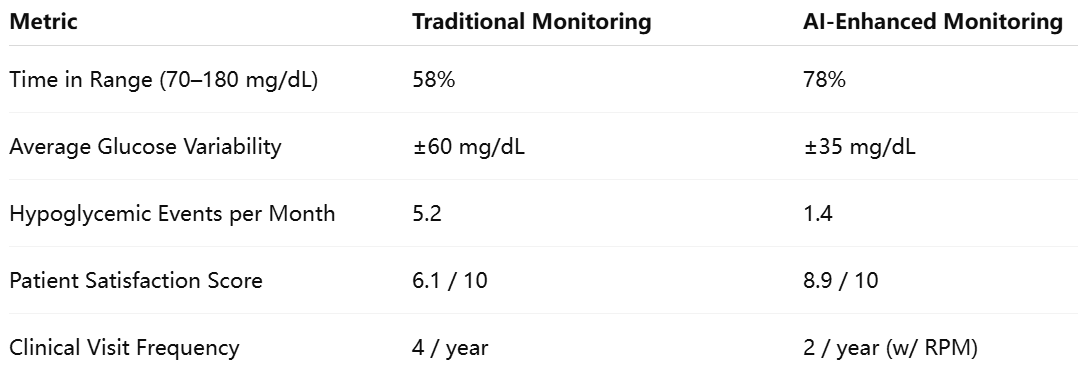
These metrics demonstrate how AI-driven forecasting not only improves medical outcomes but also enhances the patient experience and reduces the frequency of necessary clinical interactions. This dual impact—clinical efficacy and operational efficiency—positions AI as a pivotal component of modern diabetes care.
Finally, the inclusive design of the IBM-Roche system ensures that these benefits are accessible to a diverse user base. The interface is designed to accommodate varying levels of health literacy and technological familiarity, with localization options that support multiple languages and cultural dietary frameworks. These features are essential for global adoption and equity in care delivery, particularly in low-resource settings where diabetes prevalence is rising rapidly.
In sum, the clinical and consumer benefits of AI-powered blood glucose forecasting are both substantial and wide-reaching. By delivering real-time, personalized insights, the IBM and Roche system empowers individuals to take control of their health while supporting clinicians in delivering more effective, data-driven care. These advancements lay the foundation for a more proactive, patient-centered approach to chronic disease management, setting a new standard in diabetes treatment paradigms.
Challenges, Ethics, and Data Privacy in AI-Driven Diabetes Management
While the application of artificial intelligence (AI) in diabetes management brings considerable promise, it also presents a series of complex challenges, ethical dilemmas, and regulatory considerations. As IBM and Roche lead efforts in predictive blood glucose monitoring, it becomes imperative to scrutinize the limitations, risks, and obligations that accompany this technological advancement. A thoughtful approach to AI deployment is essential to ensure that such tools not only enhance healthcare outcomes but also uphold principles of fairness, transparency, and patient autonomy.
One of the primary challenges lies in ensuring the accuracy and generalizability of AI models across diverse populations. Although machine learning systems excel at detecting patterns within data, their performance is directly tied to the quality and diversity of the datasets on which they are trained. A model that performs exceptionally well in one population may falter when applied to another, especially if there are differences in age, ethnicity, diet, activity levels, or comorbidities. For instance, glucose dynamics in adolescents differ markedly from those in older adults, and individuals with Type 1 diabetes exhibit different management needs than those with Type 2. If the training data lacks sufficient representation across these dimensions, the AI system may produce biased or unreliable predictions.
Moreover, edge cases—situations that are statistically rare or deviate significantly from the norm—pose particular risks. For example, individuals with atypical metabolic responses, those on complex polypharmacy regimens, or patients with conditions such as gastroparesis may experience glucose trends that defy standard patterns. AI systems must be rigorously tested against these edge cases to minimize the risk of false positives or negatives, which could lead to incorrect interventions or a false sense of security. Validation studies must therefore extend beyond average accuracy metrics to include robustness testing in outlier scenarios.
A further area of concern involves the potential over-reliance on AI systems by both patients and clinicians. Although predictive tools can greatly assist decision-making, they should not supplant clinical judgment or patient intuition. A forecasted blood glucose drop, for instance, might prompt a patient to ingest glucose unnecessarily if it fails to materialize, leading to rebound hyperglycemia. Conversely, ignoring bodily signals in favor of digital predictions may delay appropriate interventions. Thus, it is crucial to maintain a balanced approach where AI serves as an augmentation, not a replacement, for human insight and clinical expertise.
Ethically, the deployment of AI in healthcare raises important questions related to autonomy, consent, and algorithmic transparency. Patients must be informed not only that their data is being used to train predictive models but also how those models function and influence the care they receive. The principle of informed consent must extend beyond traditional forms to include algorithmic literacy—ensuring that users understand the capabilities and limitations of the technology. Moreover, the right to opt out must be respected, and alternative care pathways must be available for those who prefer non-AI-guided interventions.
Equally pressing is the issue of data privacy and security. AI systems such as the one developed by IBM and Roche rely on the continuous collection and analysis of highly sensitive personal health data. This includes glucose levels, insulin usage, dietary intake, physical activity, and often geolocation data, especially when integrated with mobile apps. The aggregation of such data introduces significant risks if not adequately protected. Unauthorized access, data breaches, or misuse by third parties could have serious consequences, including identity theft, discrimination by insurers or employers, or psychological harm.
To mitigate these risks, the IBM-Roche platform adheres to robust compliance standards, including the Health Insurance Portability and Accountability Act (HIPAA) in the United States and the General Data Protection Regulation (GDPR) in the European Union. These regulations mandate stringent safeguards around data encryption, access control, anonymization, and data portability. However, regulatory frameworks alone are not sufficient. A proactive ethical stance—often referred to as “privacy by design”—must be embedded in the development and deployment of AI systems. This includes conducting privacy impact assessments, adopting differential privacy techniques, and ensuring that data minimization principles are followed throughout the model lifecycle.
Another key consideration is interoperability. For AI-powered systems to deliver their full value, they must integrate seamlessly with existing health infrastructure, including electronic health records (EHRs), cloud platforms, and third-party health applications. However, interoperability introduces new vulnerabilities, especially when data is shared across organizational boundaries or processed in distributed environments. Ensuring secure data exchange while maintaining functional compatibility across platforms is a technical and administrative challenge that requires ongoing investment and cross-industry collaboration.
In addition to technical and ethical concerns, there are regulatory uncertainties surrounding the classification and oversight of AI-driven medical devices. In many jurisdictions, software that performs predictive analysis and influences treatment decisions may be subject to medical device regulation. This introduces the need for rigorous clinical trials, documentation, and continuous post-market surveillance. As AI models evolve over time—either through retraining on new data or updates to the algorithmic architecture—the question arises: does a “learning” model require re-certification each time it changes? Regulatory bodies are only beginning to address these dynamic aspects of AI governance, and companies like IBM and Roche must remain at the forefront of compliance innovation.
Furthermore, there is a pressing need to ensure algorithmic fairness and equity in access to AI-powered diabetes tools. Without deliberate efforts to address health disparities, there is a risk that advanced technologies may widen the gap between well-resourced and underserved communities. For example, predictive systems that rely on continuous internet connectivity, expensive CGM devices, or smartphones may be out of reach for individuals in rural or low-income settings. Addressing this digital divide requires a commitment to inclusive design, subsidized distribution models, and partnerships with public health organizations.
Lastly, the human factor must not be overlooked. The success of AI in healthcare depends not only on technical performance but also on user trust, acceptance, and behavioral change. For predictive glucose monitoring to be effective, patients must engage with the system regularly, adhere to its recommendations, and provide accurate input data when necessary. This requires intuitive user interfaces, patient education campaigns, and responsive support channels to address concerns or misunderstandings.
In conclusion, while AI-enhanced diabetes management platforms offer unprecedented potential to improve health outcomes, they also introduce a complex array of challenges that must be addressed with diligence and foresight. The collaboration between IBM and Roche illustrates that innovation must go hand in hand with responsibility. As the healthcare industry continues to integrate AI technologies into chronic disease care, a holistic framework that balances performance, ethics, privacy, and equity will be essential to realizing the full benefits of intelligent healthcare systems.
Scaling AI in Diabetes and Chronic Disease Management
As the integration of artificial intelligence into diabetes care continues to mature, its future trajectory reveals transformative potential across healthcare systems, geographies, and patient populations. The collaboration between IBM and Roche serves as a seminal example of how AI can be used not only to manage but to anticipate chronic health conditions. The next phase in this evolution lies in achieving scale—making intelligent forecasting tools broadly accessible, economically viable, and clinically indispensable.
The scaling of AI in diabetes management is expected to follow a multi-dimensional path, encompassing technological advancement, regulatory alignment, health system integration, and patient adoption. Technologically, models will become more sophisticated, capable of incorporating increasingly diverse datasets—including genomic, microbiome, and real-time behavioral data. These inputs will enrich the predictive algorithms, improving accuracy and enabling more holistic, person-centered care. For instance, AI systems may soon account for how hormonal fluctuations, gut microbiota, or psychological stress contribute to glycemic variability, offering even more personalized recommendations.
Moreover, integration with automated insulin delivery systems is likely to expand. As AI becomes a central component in the architecture of closed-loop systems—often referred to as “artificial pancreas” solutions—it will move from a decision-support tool to a decision-execution engine. This evolution will blur the line between software and therapeutics, prompting new considerations for medical classification and oversight. The result, however, will be a major leap forward in diabetes care, where interventions become not only intelligent but fully autonomous, improving consistency, reducing human error, and alleviating the cognitive burden on patients.
Geographically, one of the most promising trends is the potential for global deployment of AI-enhanced systems, particularly in regions where diabetes prevalence is surging. Emerging markets such as India, China, Brazil, and Southeast Asia face growing epidemics of Type 2 diabetes due to urbanization, dietary shifts, and sedentary lifestyles. These regions often experience gaps in endocrinology expertise, diagnostic infrastructure, and patient follow-up. AI systems, with their ability to function remotely and at scale, can bridge these gaps by enabling early detection, personalized monitoring, and virtual care models.
However, global scaling will require careful localization. Predictive models must be adapted to reflect regional dietary patterns, language preferences, cultural norms, and healthcare infrastructure. For instance, meal-based glucose prediction algorithms must account for traditional diets such as rice-dominant or high-spice cuisine, which may influence glucose absorption differently than Western diets. Additionally, user interfaces must be translated and culturally adapted to ensure usability across different populations. IBM and Roche’s roadmap reportedly includes regional partnerships to facilitate such localization, enabling scalable deployment without compromising accuracy or user experience.
In economic terms, as adoption rises, the cost curve for AI tools is expected to decline, making them more accessible to a broader segment of the population. Already, some insurers and national healthcare systems are beginning to explore reimbursement frameworks for digital health interventions, including AI-based diabetes tools. These frameworks recognize the value proposition of AI not merely in improving quality of life but in reducing long-term healthcare expenditures through fewer complications, hospitalizations, and emergency interventions. As financial incentives align with clinical outcomes, AI tools will likely be incorporated into standard care protocols and public health programs.
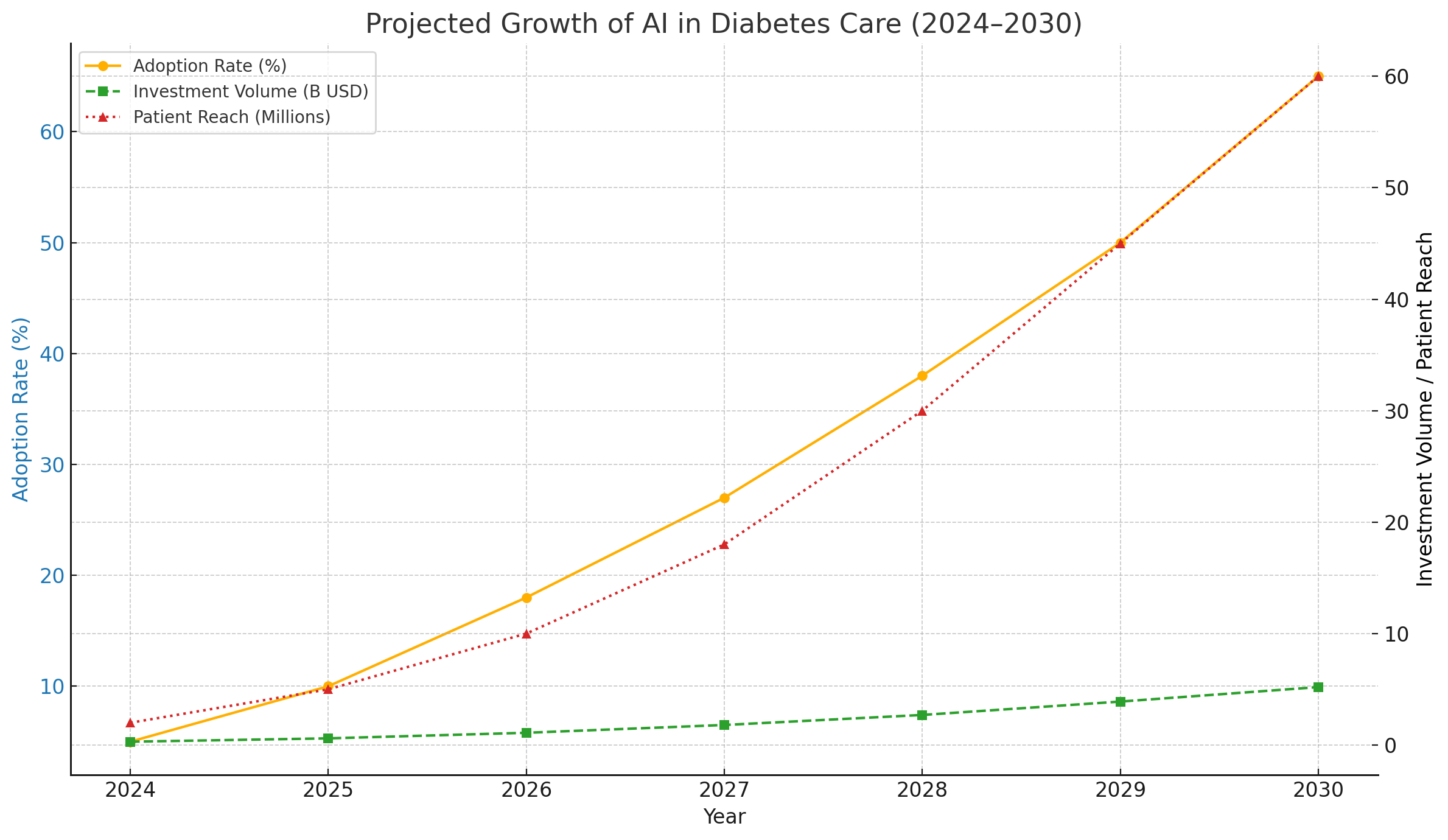
As illustrated in the chart, adoption of AI in diabetes care is expected to grow from 5% in 2024 to over 60% by 2030, with global investment exceeding $5 billion annually and patient reach projected to surpass 60 million. These numbers reflect a broader trend: the shift from episodic, reactive care to continuous, predictive, and preventive care models.
The implications extend far beyond diabetes. The architecture developed through the IBM-Roche collaboration—data aggregation, model training, prediction delivery, and user feedback loops—can be generalized to other chronic diseases such as hypertension, cardiovascular disease, asthma, and obesity. For example, AI models trained to recognize early signs of hypertensive crises or cardiac events could enable preemptive interventions, reducing morbidity and mortality rates. Similarly, behavioral data combined with pharmacological history could help optimize weight management strategies for individuals battling obesity.
In the clinical domain, AI will increasingly serve as a collaborative partner to healthcare providers. Rather than replacing medical professionals, AI will enhance their capacity to manage complex patient populations more effectively. Predictive analytics will help triage patients by risk level, identify those most likely to benefit from specific interventions, and automate routine follow-ups, allowing clinicians to focus on high-value, judgment-intensive tasks. As such, the role of healthcare professionals will evolve to include AI interpretation and digital tool stewardship, necessitating new training modules and clinical protocols.
The future will also bring more inclusive and ethical AI systems, spurred by lessons learned in early deployments. Bias mitigation techniques will be embedded into model development pipelines, and equity-focused impact assessments will become standard practice. Additionally, federated learning models—which train algorithms on decentralized data without transferring raw personal data—will help balance privacy concerns with performance optimization.
However, challenges remain. Regulatory frameworks must evolve to accommodate AI’s dynamic nature, particularly when models continuously learn and adapt in real time. Questions surrounding liability—especially in autonomous systems—will require legal clarity. And most importantly, patient trust must be maintained through transparent design, clear communication, and demonstrable results.
In the long term, AI-driven systems will contribute to a redefinition of health itself—from the absence of disease to the optimization of well-being. By continuously learning from individual and population-level data, these systems can enable truly precision-driven preventive care, offering personalized strategies for avoiding chronic conditions before they arise. For individuals already living with chronic diseases like diabetes, this shift heralds not only better clinical outcomes but a more dignified, empowered, and less burdensome health journey.
In conclusion, the future of AI in diabetes management is not a matter of potential but of execution. The foundational work laid by IBM and Roche illustrates the feasibility and efficacy of intelligent forecasting in chronic care. As technology matures, markets globalize, and ecosystems coalesce, AI will become not a luxury but a standard in healthcare. For patients, providers, and policymakers alike, the task ahead is to ensure this transformation is equitable, ethical, and centered on human health and dignity.
Conclusion: Human-Centric AI for Better Health
The integration of artificial intelligence into diabetes management, as exemplified by the pioneering collaboration between IBM and Roche, signals a fundamental shift in how chronic diseases are understood, monitored, and treated. By transforming raw data into predictive intelligence, AI has moved diabetes care beyond static, reactive routines toward a dynamic, anticipatory model rooted in personalization and prevention.
At the heart of this innovation is a recognition that managing diabetes is not solely a medical task—it is a daily challenge that intersects with lifestyle, behavior, environment, and emotion. Traditional tools, while essential, have often fallen short of empowering individuals to navigate this complexity with confidence and clarity. AI addresses this gap by offering real-time foresight, contextualized recommendations, and adaptive learning that evolves with the user.
Yet, technology alone is not enough. The future of AI in healthcare must remain deeply human-centric. This means prioritizing transparency, respecting privacy, ensuring equitable access, and building trust through explainable and inclusive systems. It also means designing tools that augment, rather than replace, the irreplaceable intuition and care of human clinicians.
The road ahead holds immense promise. With continued advancements in data science, device integration, regulatory frameworks, and patient engagement, AI-powered platforms will become not only more accurate but more accessible. As adoption expands globally, they will enable millions of people—not just to manage diabetes—but to live more freely and fully despite it.
In this broader vision, AI becomes more than a technological achievement; it becomes a tool for human flourishing. When designed with empathy, deployed with integrity, and scaled with foresight, AI can reshape chronic disease care into a system that is not only smarter—but kinder, more responsive, and more just.
The future of healthcare lies not only in what machines can do, but in how they help people live better. Diabetes management is just the beginning.
References
- Roche and IBM Collaborate on AI-Driven Diabetes Management
https://www.roche.com/media/releases/med-cor-2020-09-01.htm - IBM Watson Health: Transforming Chronic Disease Care
https://www.ibm.com/watson-health/learn/chronic-disease - Mayo Clinic: Managing Blood Sugar in Diabetes
https://www.mayoclinic.org/diseases-conditions/diabetes/in-depth/blood-sugar/art-20046628 - American Diabetes Association – Standards of Medical Care
https://diabetes.org/diabetes/technology/standards-of-care - FDA Guidance on Artificial Intelligence in Medical Devices
https://www.fda.gov/medical-devices/software-medical-device-samd/artificial-intelligence-and-machine-learning-samd - World Health Organization: Global Diabetes Data and Trends
https://www.who.int/news-room/fact-sheets/detail/diabetes - Health Affairs: The Future of AI in Chronic Disease
https://www.healthaffairs.org/do/10.1377/forefront.2023 - Nature Digital Medicine: Explainable AI in Clinical Practice
https://www.nature.com/articles/s41746-018-0021-1 - IEEE Spectrum: AI-Powered Insulin Delivery Systems
https://spectrum.ieee.org/artificial-pancreas-diabetes - McKinsey & Company: Scaling AI in Healthcare Systems
https://www.mckinsey.com/industries/healthcare/our-insights/scaling-ai-in-healthcare